Paediatric Sepsis – Fluid management

Early intervention and treatment for children with sepsis
It is well documented that quick intervention improves outcomes for sepsis patients1. Yet, severe sepsis continues to be a major cause of morbidity and mortality among children, with septic shock responsible for 10–25% of Paediatric Intensive Care Unit (PICU) admissions worldwide2. Hon et al highlights, “early treatment with antimicrobial therapy, fluid therapy and vasoactive medications, and rapid recognition of the source of sepsis and control are the key recommendations from paediatric sepsis management guidelines3”. However, deciding on the appropriate therapy required for sepsis cases can potentially add precious time to the treatment timeline for these vulnerable patients; therefore, when minutes matter Mostcare Up enables your team to make better decisions faster.
When Minutes Matter: Early detection, early prevention.
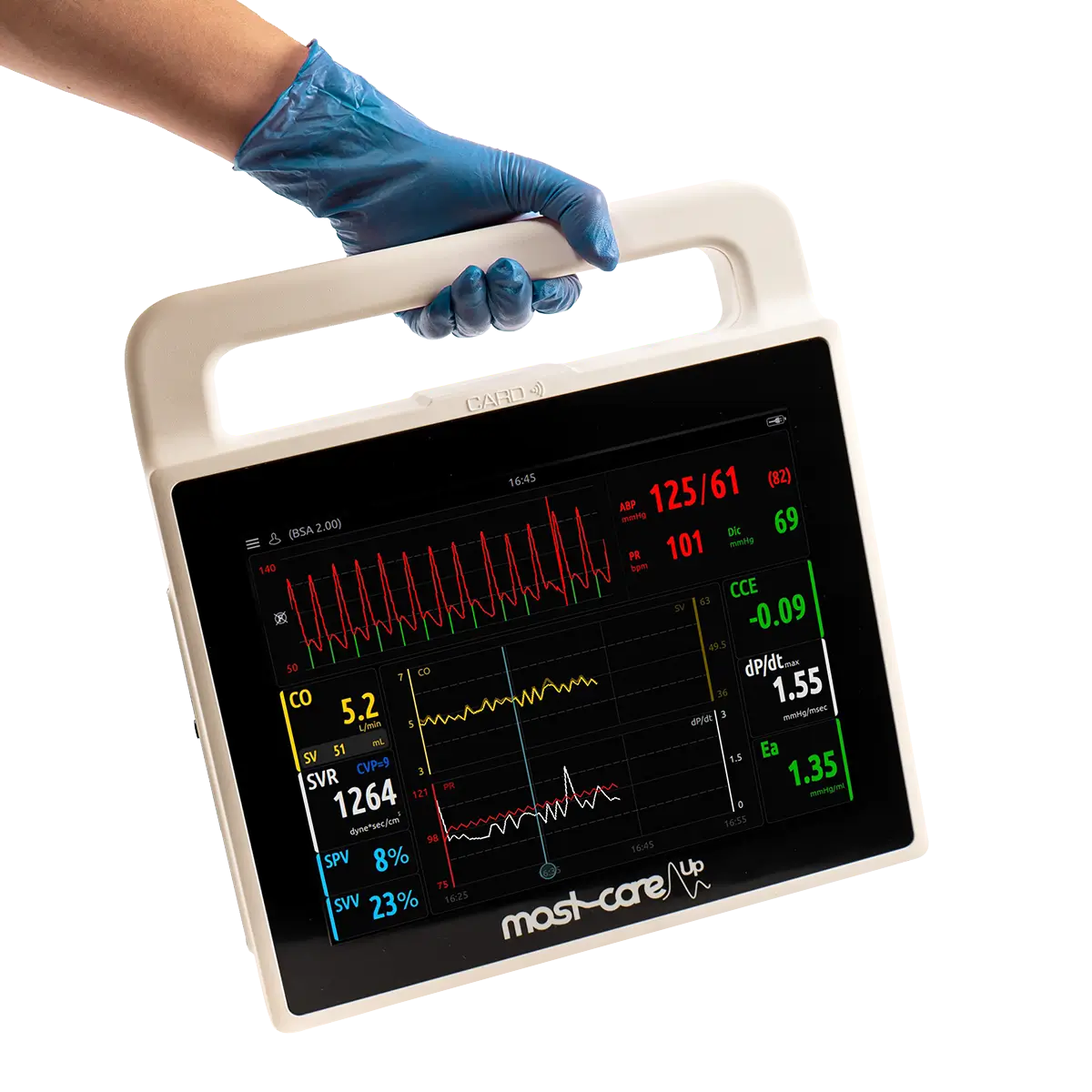
The goal of therapy is to de-escalate septic shock; therefore, choosing the correct therapy is a crucial and time-sensitive decision. The necessity to continually monitor paediatric patients with sepsis is critical, especially if the patient enters sepsis shock, which can rapidly cause cardiac depression with cardiac output. However, not all monitors provide the same data and visibility to make those quick decisions.
“…Septic shock and multiple organ dysfunction syndrome are the most critical groups which account for a high mortality rate in paediatric sepsis, and their clinical course often deteriorates rapidly. Resuscitation based on haemodynamics can provide objective values for identifying the severity of sepsis and monitoring the treatment response.”4
When vital signs drop, instant intervention is required. However, if you’re unable to understand the cause of the drop, it’s difficult to know the proper treatment plan to implement. Do you provide fluids or medicine? Those precious minutes waiting to see if the medicine is working can have serious ramifications. On the other hand, administering too much fluid can become hazardous. Because fluids will accumulate in various body tissues including the lungs and the liver with changes detected clinically only after the patient had already received extra fluids and lost a valuable time in the critical initial window for the management of shock5. These extra fluids will also extend the patient's time on mechanical ventilation, PICU length of stay, and increase the risk of morbidity and mortality5.
Therefore, it’s imperative clinicians and medical teams have better visibility into the breakdown of output data to be able to make better, faster, decisions leading to better treatment.
“Optimization of advanced haemodynamics, such as cardiac output and systemic vascular resistance, has now been endorsed as better therapeutic guidance for sepsis.”4
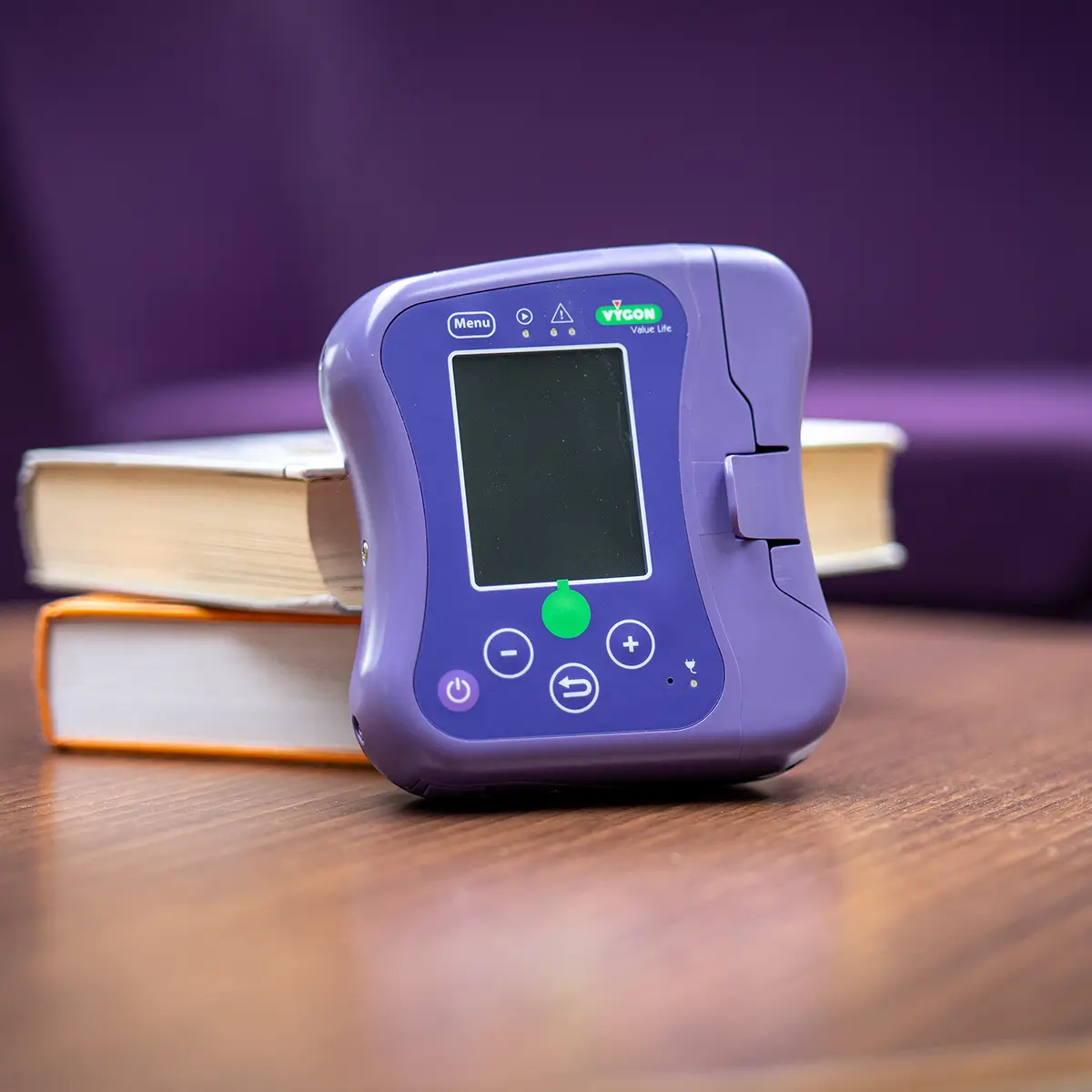
Our solution? Mostcare Up not only provides a clear illustration of what therapy might be necessary but provides a beat-by-beat picture of the effectiveness of the given treatment.
Mostcare Up: Haemodynamic monitoring for paediatrics
When assessing the benefits of Mostcare Up, the value for paediatrics cannot be overlooked, especially in sepsis cases. With insights to provide better fluid management, the overall benefits of Mostcare Up are universal. The only haemodynamic monitor validated for both adults and paediatric patients using the PRAM algorithm that provides 1,000 data points with beat-by-beat insight, Mostcare Up’s visibility enables clinicians to act quickly.
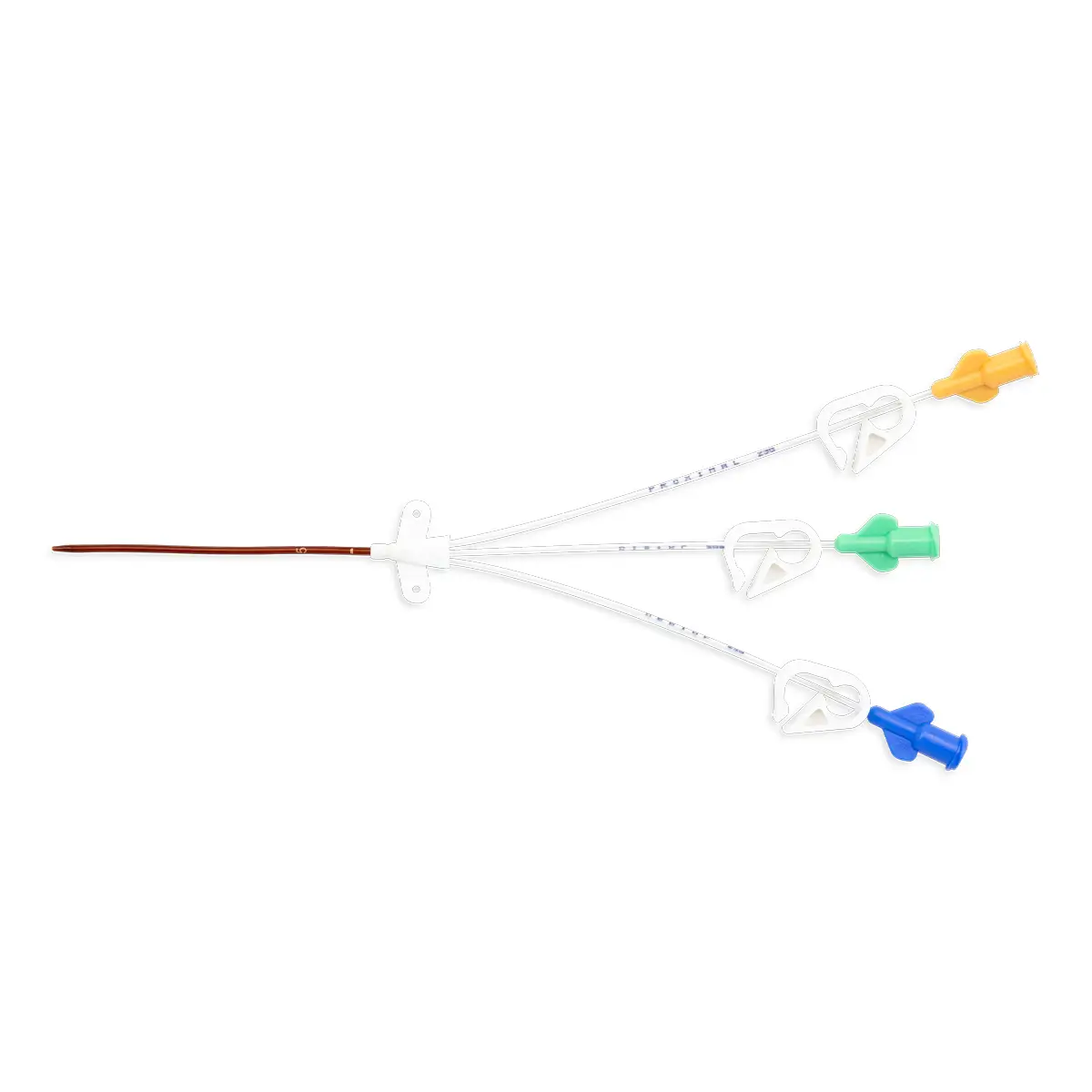
In a comparative study by Calamandrei et al, it’s stated that “haemodynamic monitoring is fundamental to the management of the critically ill paediatric patient, but clinical estimation of cardiac output (CO) in children has been shown to be inaccurate. The need to monitor cardiac function is underlined by the fact that a low flow state carries a higher mortality in septic shock”6.
The same study concludes that in the range of ages evaluated, PRAM provides reliable estimates of cardiac output when compared with non-invasive techniques6.
See also: Cardiac Output monitoring in children: supporting practice to make informed decisions.

For sepsis intervention, the benefits of Mostcare Up could be life-changing for paediatrics. The pre-set parameters target individual waveforms, rather than depending on pre-estimated metrics from a database, offering unique visibility to the specific patient.
In addition, further benefits for the patients and the practice include:
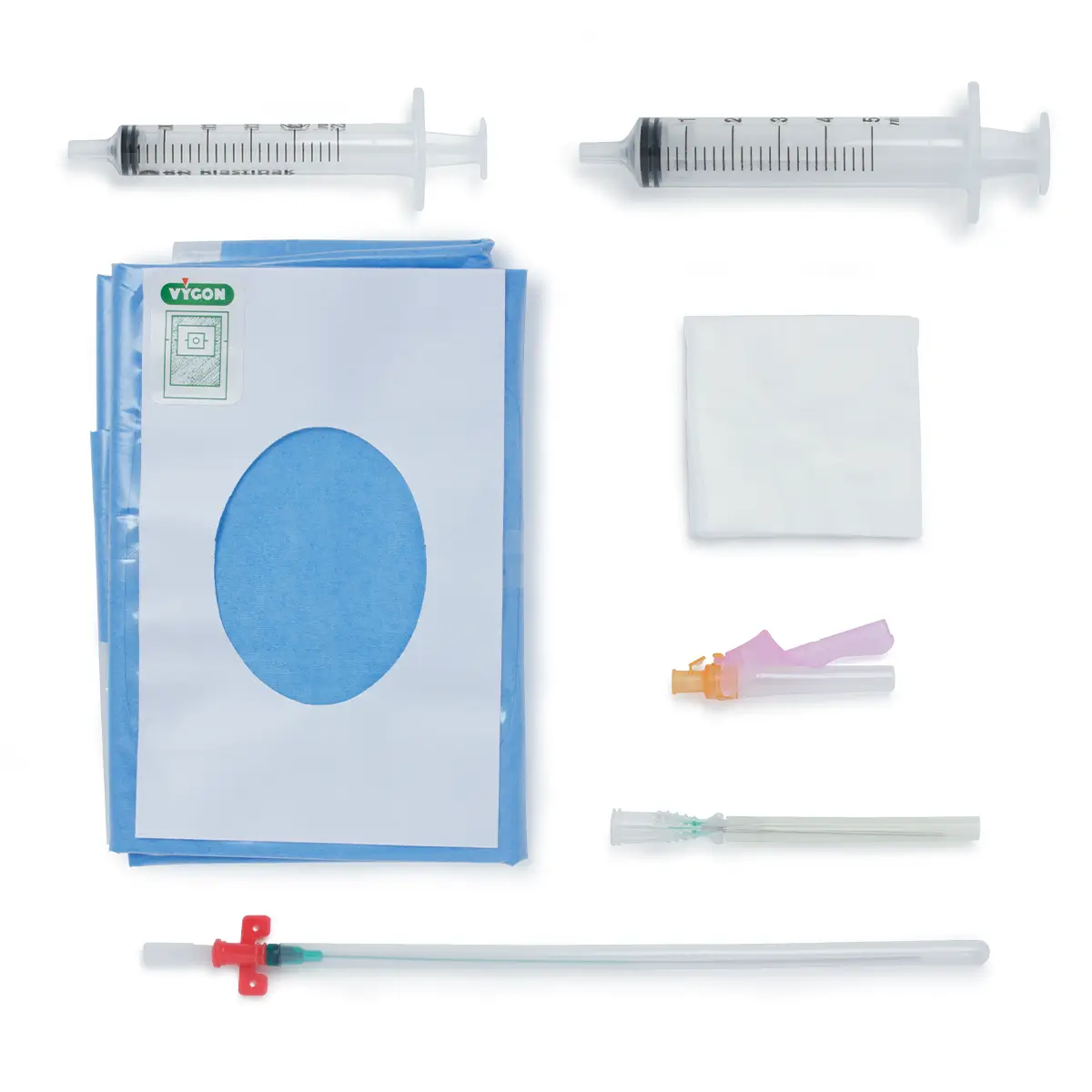
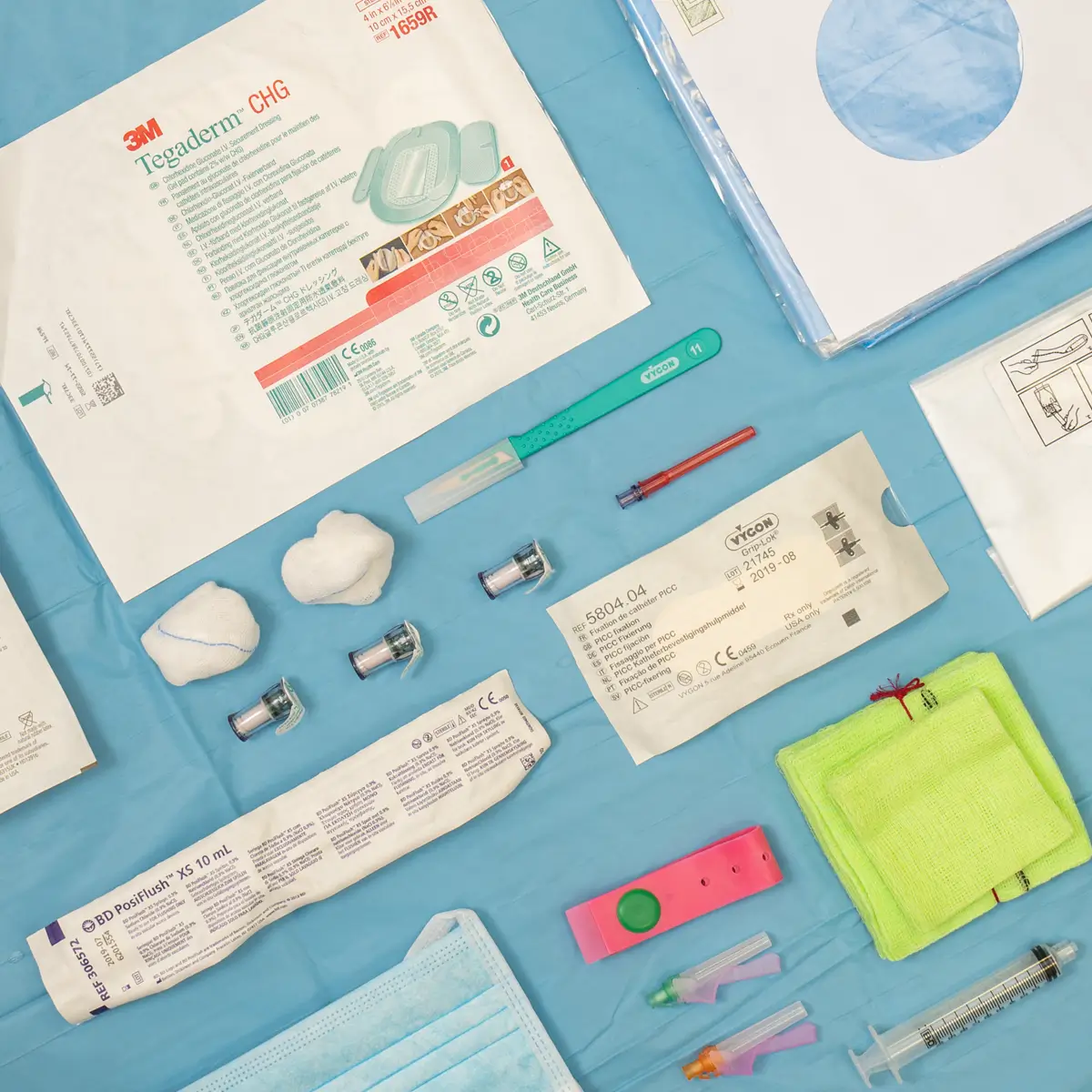
No consumables: This means medical teams are not limited to a set number of uses with Mostcare Up (and can be used on multiple patients with no extra costs associated). Therefore, no hesitancy when deciding if/or not, to utilise the machine due to use restrictions on similar devices, nor lost valuable time in critical moments locating a device access card to start the machine.
Quick simple setup: plug in and go, no wasted time as Mostcare Up has a 60-second setup.
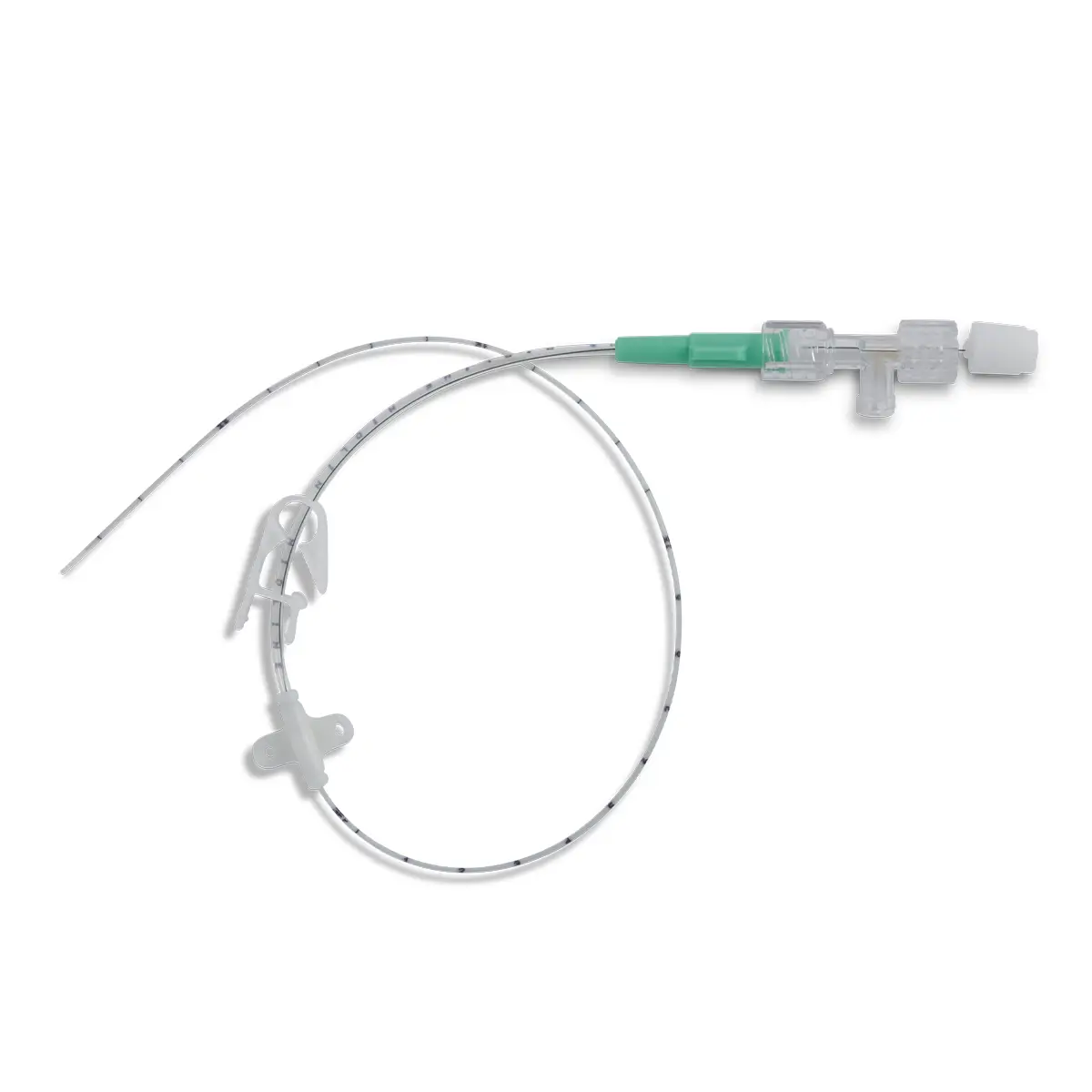
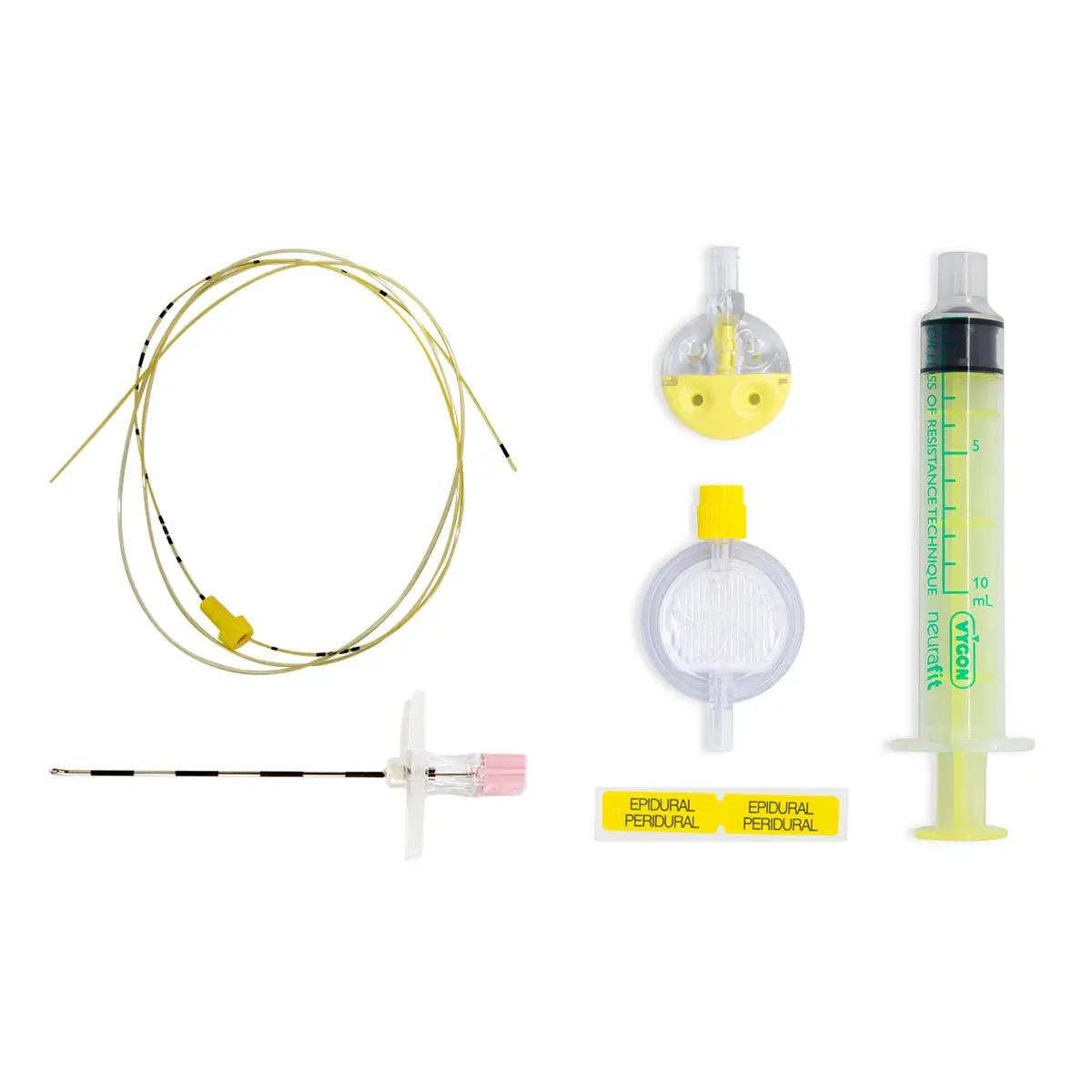
Minimally invasive device: Can be used on patients before they become critical as a preventative measure.
PRAM Algorithm: The only algorithm validated for use in paediatrics 7.
The fluid management and ability to make quick decisions are at the heart of the monitor. However, subsequential benefits hospitals have experienced using Mostcare Up have resulted in a reduced length of stay, reduced costs associated with treatment and greater insights into providing therapy resulting in better patient outcomes.
“Before using the [Mostcare Up] monitor our fluid therapy involved giving medication during the procedure to manage blood pressure, with the monitor we can give better fluid levels which reduces the need for more medication.8” – Rocio Occia Ferrao, Consultant, NNUH
Arrange an evaluation in the field and see the benefits.
Ongoing service and support from Vygon
In addition to our technical team and onsite lab providing ongoing technical support, we have a team of Clinical Nurse Advisors, including two Haemodynamic Specialists, who are on hand to support your hospital or trust.