Cardiac Output monitoring in children: supporting practice to make informed decisions.

“We suggest using advanced hemodynamic variables, when available, in addition to bedside clinical variables to guide the resuscitation of children with septic shock or other sepsis associated organ dysfunction.”
Surviving Sepsis Campaign International Guidelines for the Management of Septic Shock and Sepsis-Associated Organ Dysfunction in Children, Ped Crit Care Med. 2020 Feb
Early and appropriate fluid administration is vital in children, as it has been proven to improve outcomes and reduce mortality[2].
Sepsis continues to be a leading cause of morbidity and mortality among children, with septic shock responsible for 10–25% of Paediatric Intensive Care Unit (PICU) admissions worldwide[3].
Fluid administration is one of the recommended treatments for children with severe sepsis. Early recognition, early administration of antibiotics, and early reversal of the shock state with aggressive fluid resuscitation and administration of vasoactive medications are all part of the ‘golden hour’ of trauma resuscitation.[4] However, fluid resuscitation within this demographic is moving away from exact volumes from a set protocol and starting to develop into a more personalised approach where the clinical markers of fluid responsiveness are monitored.
Current methods of haemodynamic monitoring
The most common form of haemodynamic or cardiac output monitoring is Echocardiography, which has become an indispensable bedside diagnostic tool in the realm of paediatric intensive care units (PICUs). Echo cardiac output monitoring has proven to be an influential factor in the formula of clinical decision-making. [5]
However, Echo has its limitations; the measurements are taken at one point in time, giving a snapshot of the patient’s condition rather than monitoring changes in the patient condition over time; training is required to operate the machine as well as time to interpret the images, this can cause delays to monitoring while waiting for the appropriate staff.
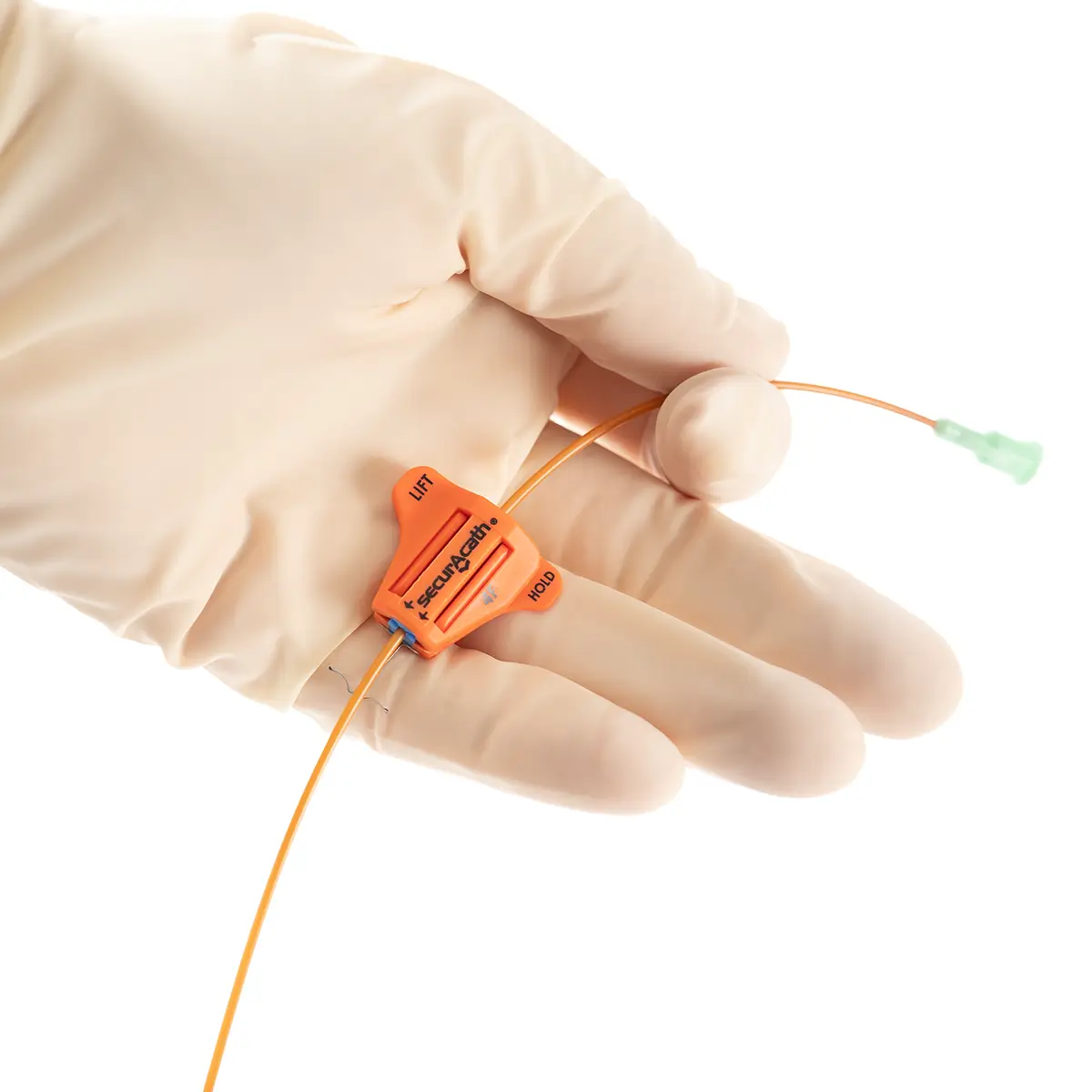
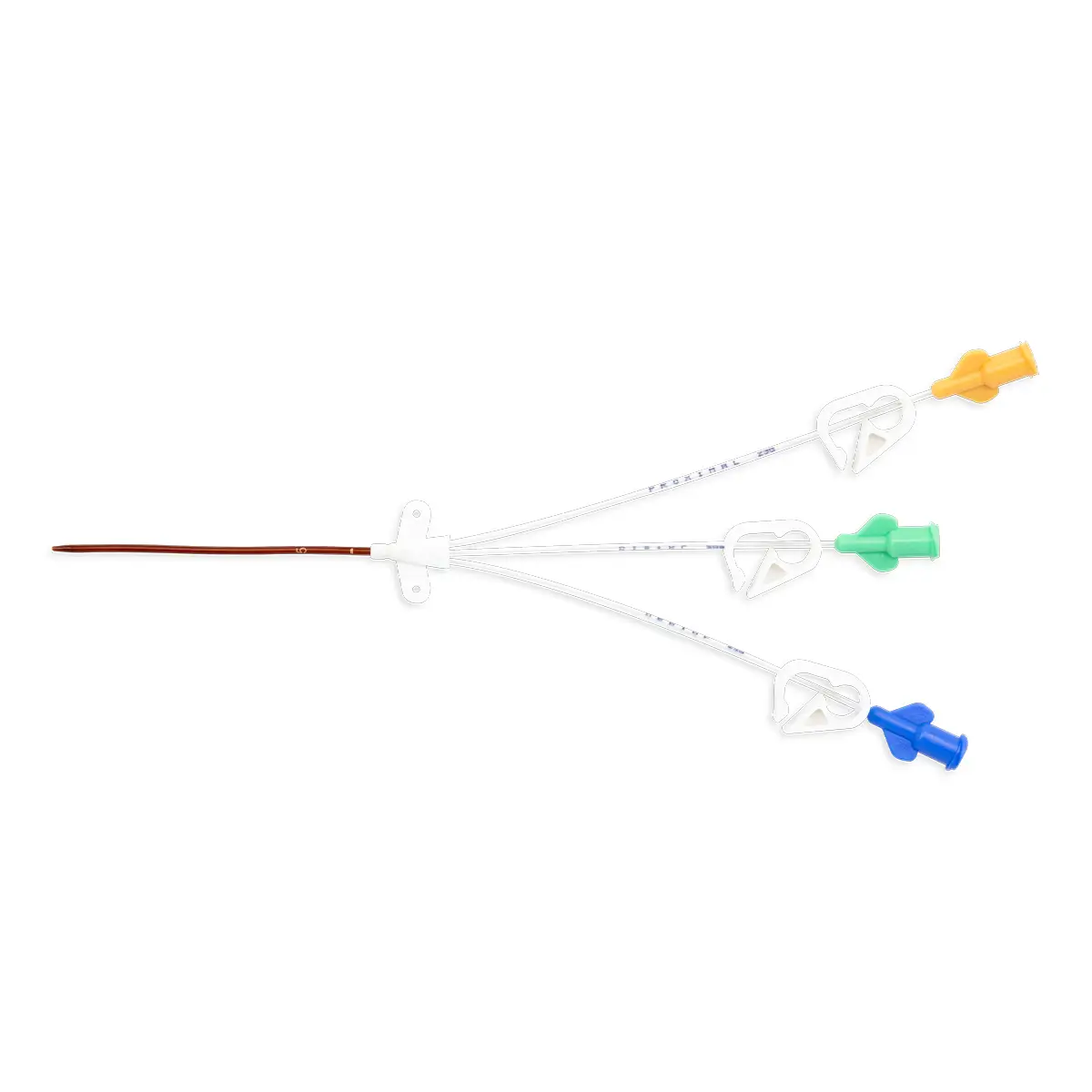
Pulse contour methods of cardiac output monitoring can be used as a complimentary form of monitoring to Echocardiography. By providing continuous monitoring of the patient in real-time, clinicians can utilise trend data to support practice and make informed decisions. This can lead to earlier intervention which improves the patient outcomes.
Pulse contour monitoring
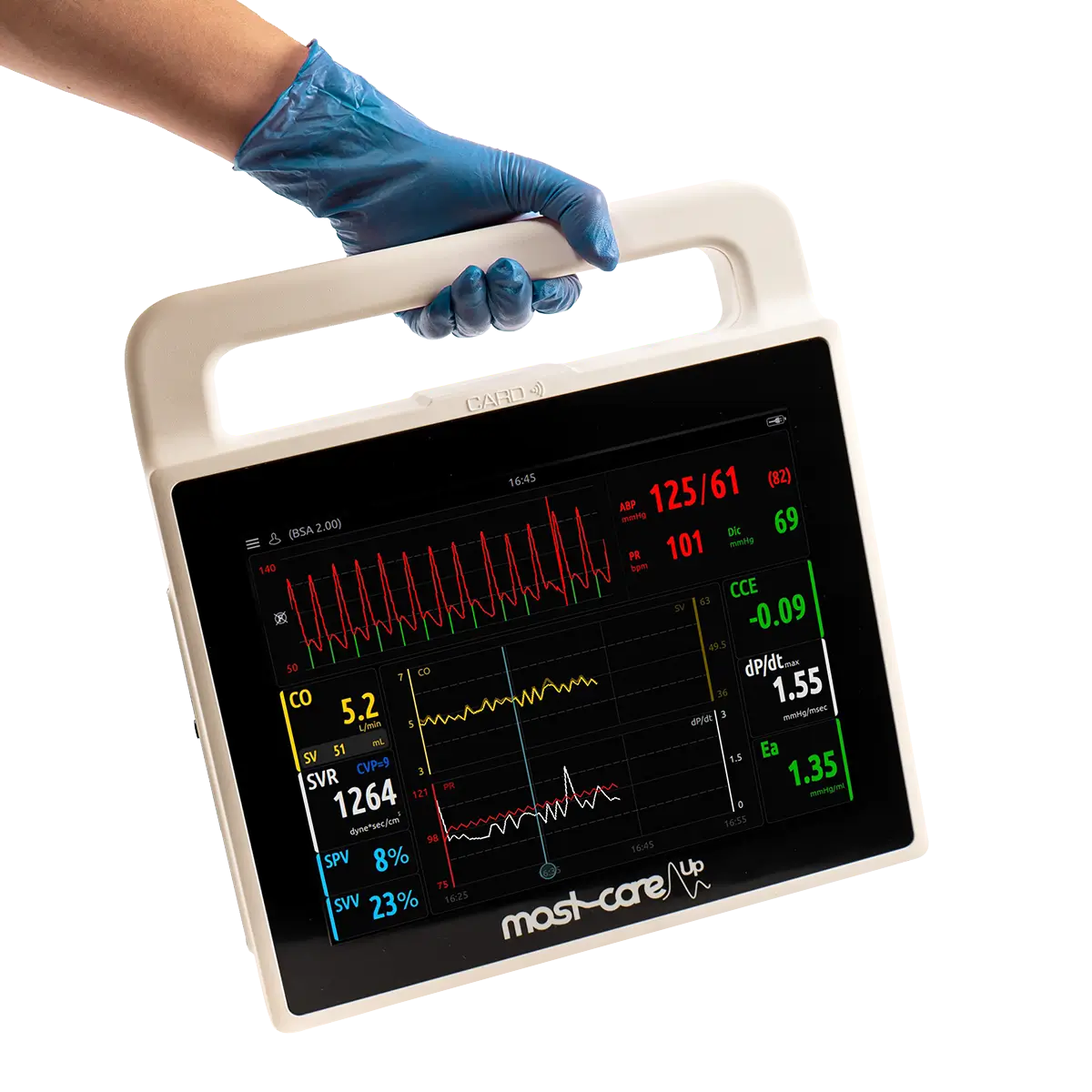
Pulse wave analysis allows an estimation of cardiac output based on continuous analysis of the arterial blood pressure waveform, a complex physiological signal determined by an interplay of left ventricular stroke volume, systemic vascular resistance, and vascular compliance.[6]
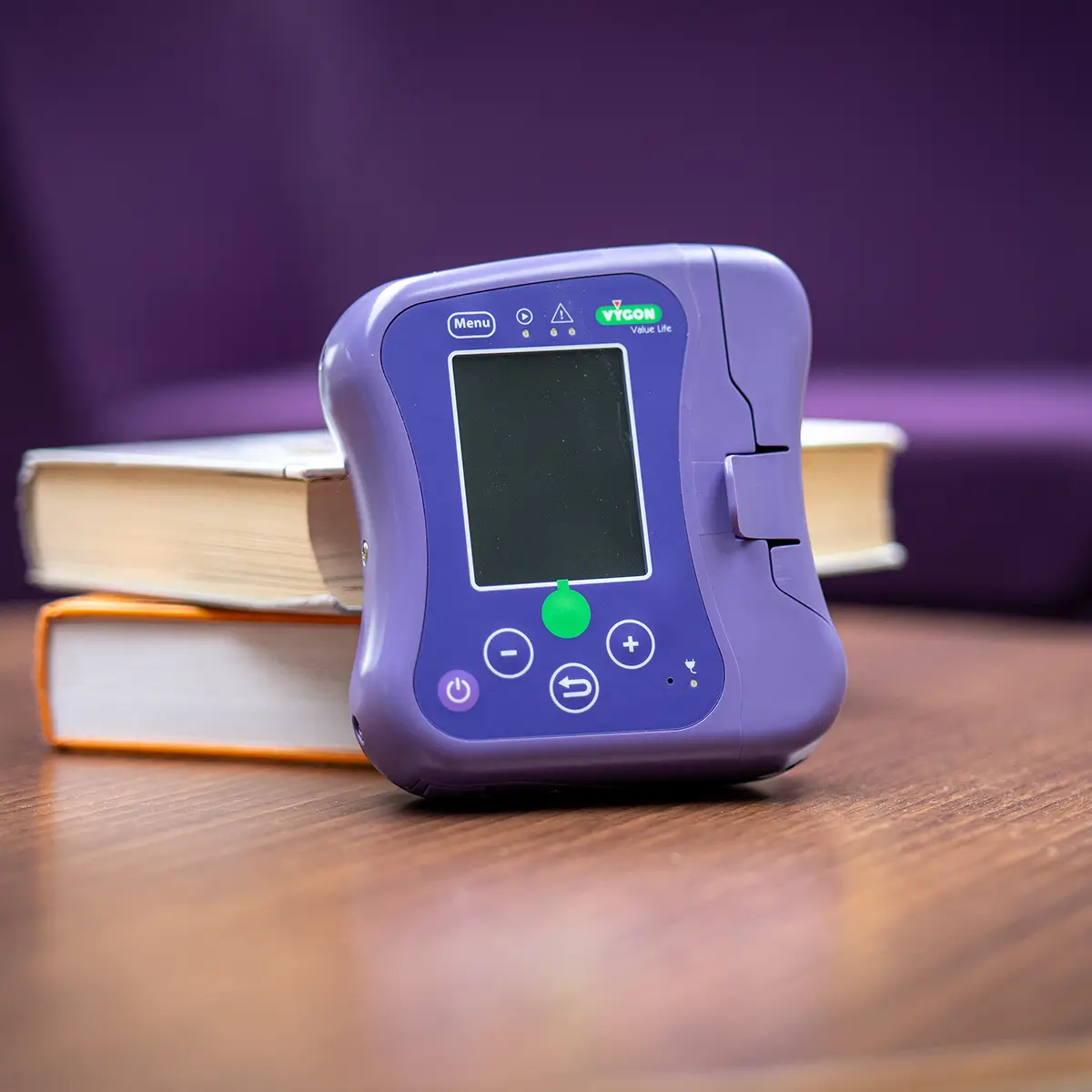
Mostcare UP is the only pulse contour cardiac output monitor validated for use in paediatrics. It can be set up in three easy steps and doesn’t require consumables, benefiting unlimited patient usage and improving sustainability.
Mostcare UP can display trends for many haemodynamic variables simultaneously and allows for constant and sensitive monitoring in real time of the slightest haemodynamic variations.
- Sampling at 1,000Hz
- Beat-by-beat analysis of the waveform
- Does not depend on pre-estimates
- No external calibration required.
- HL7 compatible for data transfer
Used alongside existing practice, Mostcare UP enables clinicians to make more informed decisions.
96% of first-time users agree or strongly agree that Mostcare UP is easy to use.
Training & support
We deliver a personalised ongoing training package to support your needs. We are proud to have Haemodynamic Specialists in the Vygon Critical Care team. As highly accomplished specialists in their fields, our Haemodynamic Specialists offer a premium level of valuable support. The level of detail and skill in our implementation training packages ensures that our Haemodynamic Specialists are able to guide clinicians and clinical teams from evaluation to adoption and beyond.
Arrange an evaluation in the field and see the benefits.