Fluid therapy: The risk of fluid overload

It's clear that fluid management is a critical aspect of patient care, especially in conditions like septic shock where the balance between administering enough fluids to support the patient and avoiding fluid overload is delicate. Administering fluids carries certain risks that healthcare providers need to be aware of and manage appropriately.
Here's a breakdown of the concerns related to fluid overload and some strategies to prevent it:
Complications of Fluid Overload:
Organ Dysfunction: Too much fluid can lead to increased stress on the heart, lungs, and other organs, potentially worsening their function. It can also impair tissue oxygenation by increasing interstitial pressure and limiting blood flow to tissues.
Respiratory Complications: Excess fluid can accumulate in the lungs, causing pulmonary edema and compromising gas exchange. This can result in respiratory distress and hypoxia.
Cardiovascular Strain: Overloading the cardiovascular system can lead to increased workload on the heart, potentially contributing to cardiac dysfunction and even heart failure.
Delayed Recovery: Fluid overload can lead to prolonged recovery times, increased hospital stays, and overall poorer patient outcomes.
It is important to keep in mind that fluids are drugs and treatment should include every effort to reduce harm. Fluids should only be prescribed when they are clearly indicated and should balance the risk of not administering enough with the increasingly apparent risks of too much fluid.
Their characteristics, indications and contraindications should be carefully considered when choosing their type, their dose, the timing of their administration and the timing for their removal.
Preventing Fluid Overload:
Experts’ opinion:
We propose to routinely use a personalized approach of intraoperative fluid infusion/volume expansion based on the individual hemodynamic response to volume titration to reduce the deleterious side effects of fluids and improve patients’ outcome (agreement 100%)1
Adopting a personalised approach to fluid management is crucial. This involves monitoring each patient's individual response to fluid administration and adjusting the infusion rates accordingly. This can help avoid unnecessary fluid administration in patients who might not need it.
Early Goal Directed Therapy: This approach involves using specific haemodynamic goals to guide fluid administration and other interventions. It focuses on optimising cardiac preload, afterload, and contractility to match oxygen delivery with the patient's oxygen demand. This can help avoid both under-resuscitation and fluid overload.
Dynamic Monitoring: Using dynamic parameters, such as stroke volume variation or pulse pressure variation, can provide real-time information about fluid responsiveness. These parameters help clinicians make informed decisions about whether a patient will benefit from additional fluids.
Strict Monitoring: Frequent monitoring of the patient's vital signs, fluid input/output, and clinical status is essential to detect early signs of fluid overload. This allows for timely interventions to prevent its progression.
The Solution:
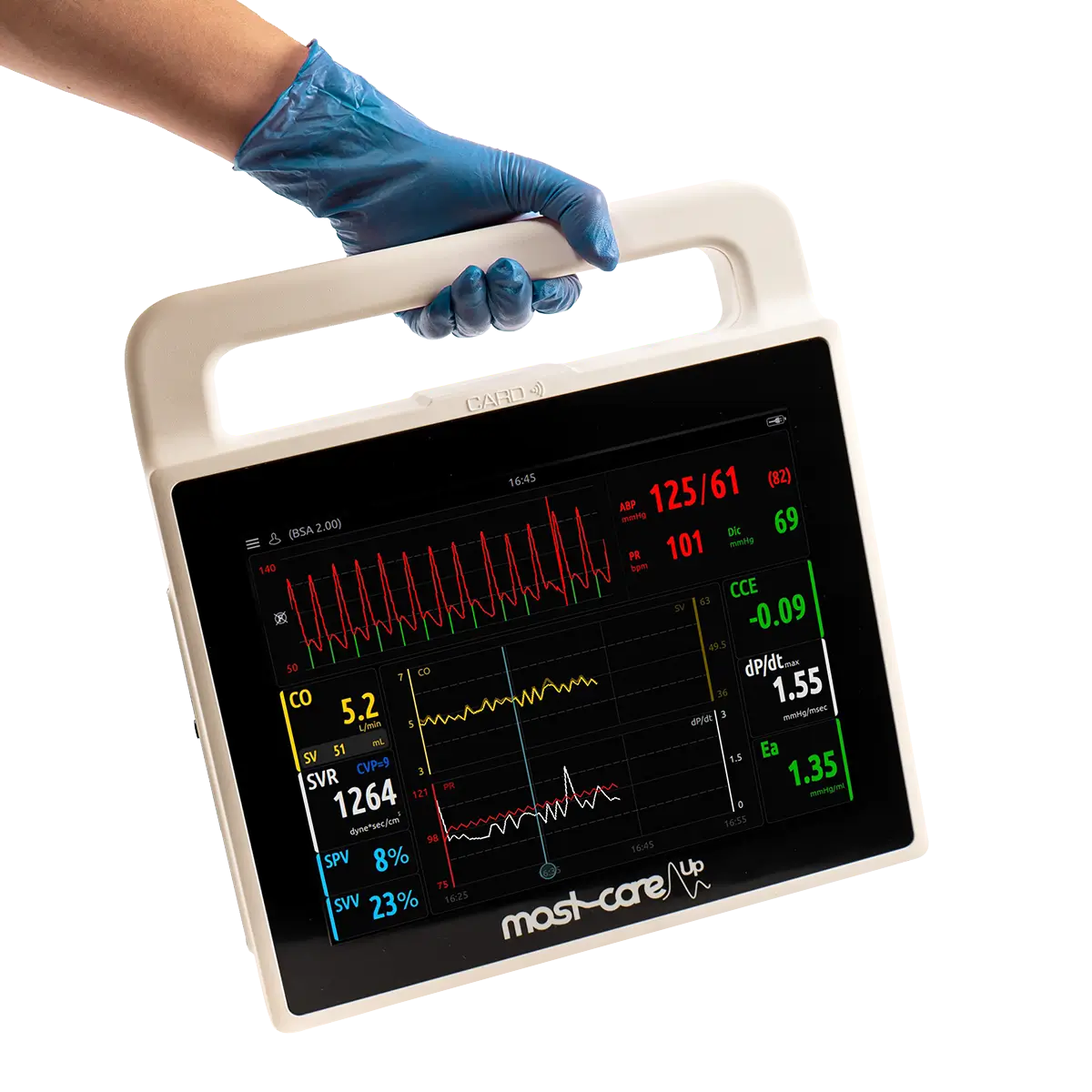
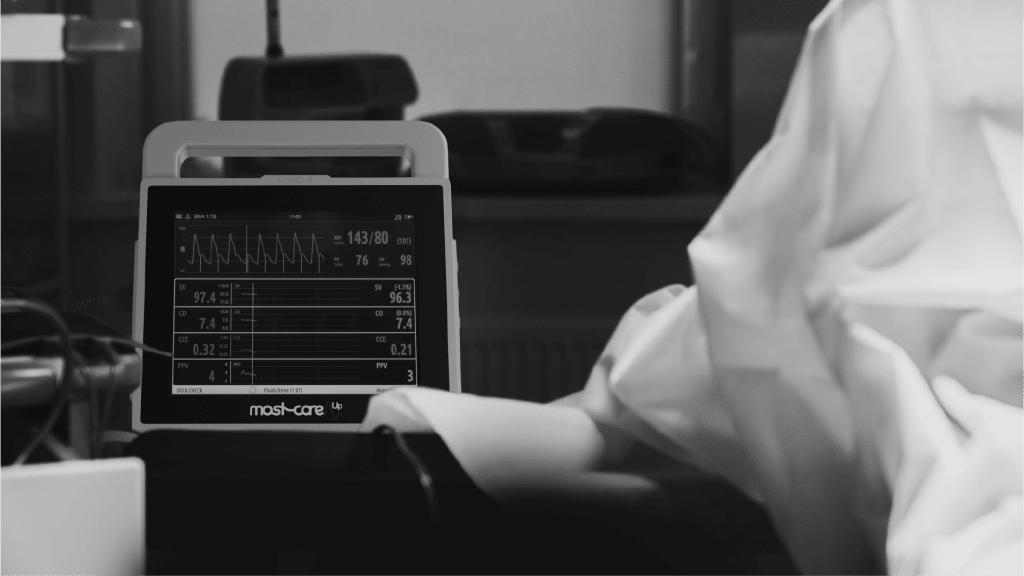
Mostcare Up is a minimally invasive haemodynamic monitoring system designed to provide real-time information about a patient's haemodynamic status, allowing clinicians to make informed decisions regarding fluid management, cardiovascular performance, and other critical aspects of patient care.
Clinicians can use various parameters to assess the patient's haemodynamic status, including cardiac output, stroke volume, systemic vascular resistance, and more. By continuously monitoring these parameters, healthcare providers can tailor fluid administration, vasopressor therapy, and other interventions to optimise the patient's cardiovascular function.
This technology aims to improve patient outcomes by helping clinicians avoid both inadequate fluid resuscitation and excessive fluid administration, which can lead to complications such as fluid overload. It's particularly useful in situations where patients are at risk of hemodynamic instability, such as those undergoing surgery, in the intensive care unit, or with conditions like septic shock.
In essence, the key is finding the right balance between providing adequate fluid resuscitation to support the patient's needs and avoiding the harmful consequences of fluid overload. This requires a multidisciplinary approach, close patient monitoring, and the ability to adjust fluid administration based on the patient's evolving condition.
If you want better patient outcomes, speak to us about Mostcare Up today.
Trial Mostcare in your Department
Despite all the clinical evidence, it's always best to see the benefits for yourself. At Vygon, we support with evaluations in your department and training staff so you can discover for yourself how Mostcare UP would help your patients and team.
Experience the benefits for yourself with an evaluation in your hospital.
Training & knowledge
Vygon can help support your department in integrating Mostcare Up. We have Clinical Haemodynamic Specialists available to train your team while they work, supporting practice and informed escalation.
References:
[1]Perioperative hemodynamic optimization: from guidelines to implementation-an experts' opinion paper. Fellahi JL, Futier E, Vaisse C, Collange O, Huet O, Loriau J, Gayat E, Tavernier B, Biais M, Asehnoune K, Cholley B, Longrois D. Ann Intensive Care. 2021 Apr 14;11(1):58. doi: 10.1186/s13613-021-00845-1. PMID: 33852124; PMCID: PMC8046882.
[2]Early Goal-Directed Therapy in the Treatment of Severe Sepsis and Septic Shock Emanuel Rivers, M.D., M.P.H., Bryant Nguyen, M.D., Suzanne Havstad, M.A., Julie Ressler, B.S., Alexandria Muzzin, B.S., Bernhard Knoblich, M.D., Edward Peterson, Ph.D., and Michael Tomlanovich, M.D. for the Early Goal-Directed Therapy Collaborative Group*
[3]Goal directed fluid therapy decreases postoperative morbidity but not mortality in major non-cardiac surgery: a meta-analysis and trial sequential analysis of randomized controlled trials. Som A, Maitra S, Bhattacharjee S, Baidya DK. J Anesth. 2017;31:66–81.
[4]Principles of fluid management and stewardship in septic shock: it is time to consider the four D’s and the four phases of fluid therapy. Malbrain, M.L.N.G., Van Regenmortel, N., Saugel, B. et al. Ann. Intensive Care 8, 66 (2018). https://doi.org/10.1186/s13613-018-0402-x