Choosing a Needle Free Connector

There are many different varieties and options available on the market which can make the selection of a new device into a trust and/or department a difficult process. In this article we uncover 10 key criteria and considerations to acknowledge when looking to introduce a needle free connector.
(5-10 min read)
- What is a needle free connector
- 10 Key Criteria
1. Microbial Ingress Testing Data
2. Split Septum VS Mechanical Valve Devices
3. Fluid displacement options
4. Device and Septum Disinfection
5. Biofilm reduction
6. Fluid pathway considerations
7. Clamping sequence requirement and standardisation
8. Device Design
9. Compatibility with drug interaction and other IV Connections
10. Benefits to patients and staff - Needless connector solutions from Vygon UK
- Total Solutions
- Article References
What is a Needle Free Connector?
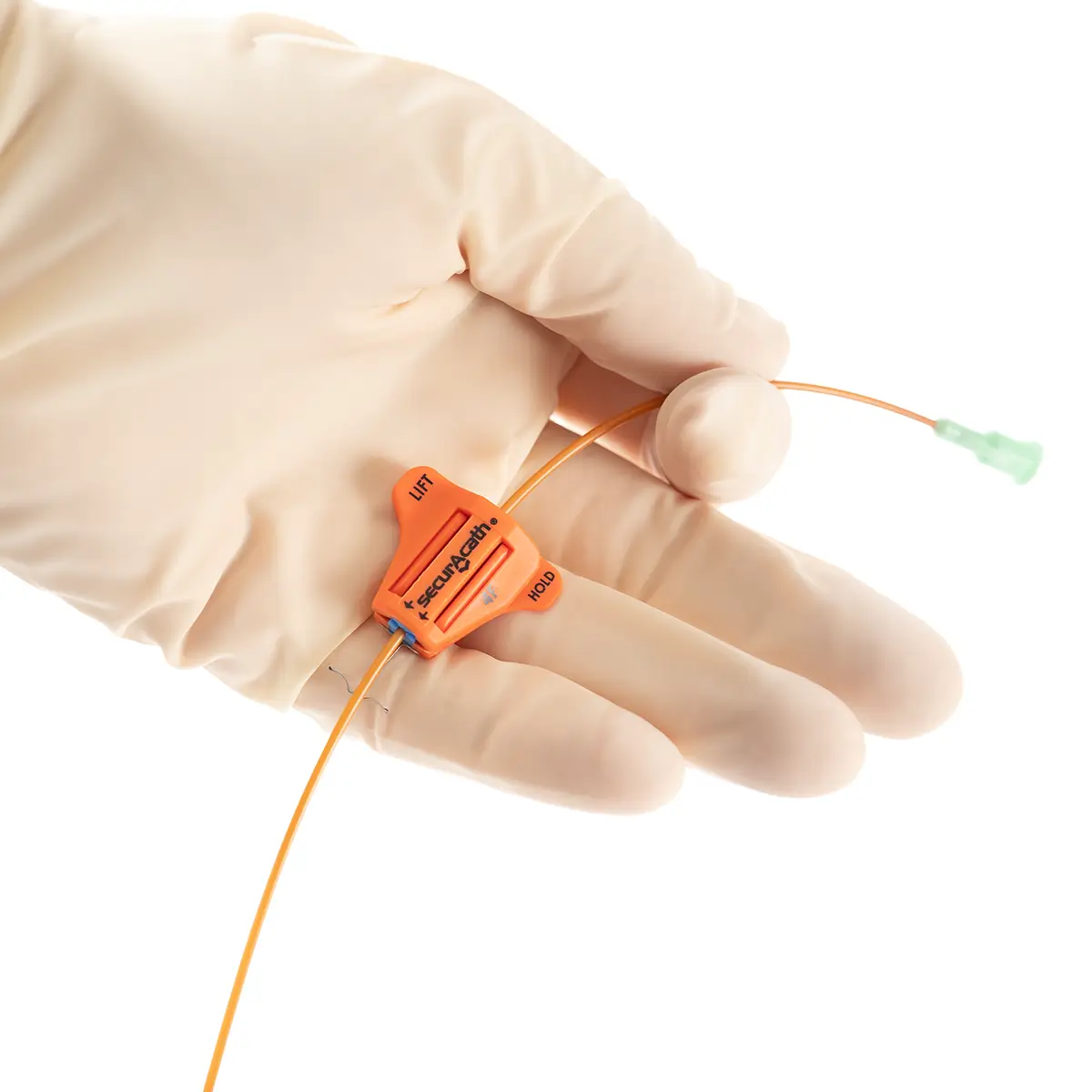
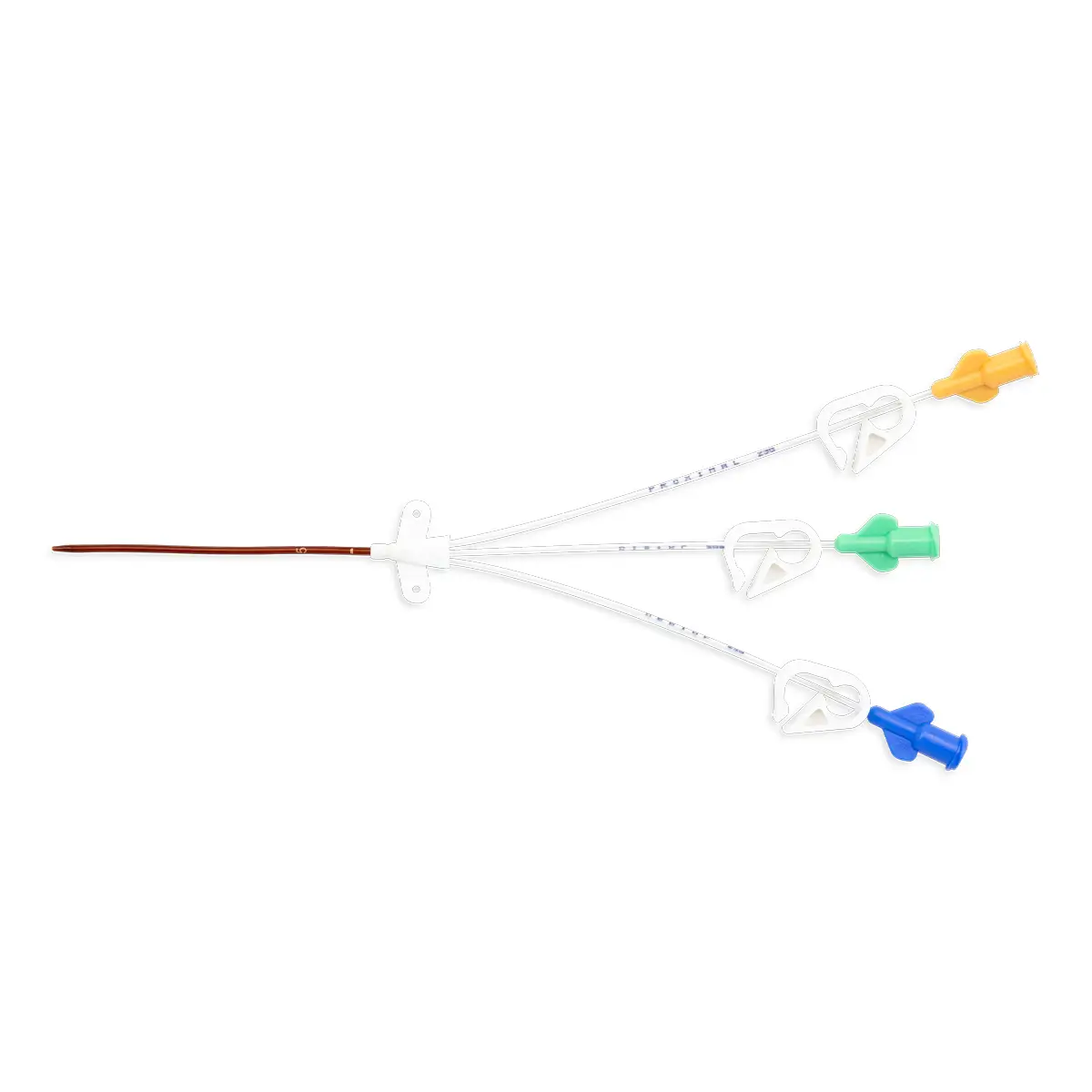
Put simply, a needle free connector is an essential device that connects to the end of a vascular access device (VAD), catheter/cannula extension set, to enable catheter access for injection, infusion, or aspiration.
Using a needle free connector reduces the risk of occlusion, microbial and/or water ingress, or seepage from the catheter or cannula. It also requires no needle for access thus preventing the associated risk of a needlestick injury (NSI).
10 Key Criteria and Considerations when Selecting a Needle Free Connector for your Trust
When it comes to selecting a needle free connector, the variety available within the market can make this purchasing and clinical decision challenging. “There are various different designs which potentially may make it difficult for purchasers to identify the features which present the least risk and greatest safety.”(26).
When next reviewing your needless connector solution for your trust, use the below 10 criterium to help you and your trust make the most informed purchasing decision.
Microbial Ingress Testing Data
Ensure your needle-free connector is supported by microbial ingress testing data. (1) This will be available from your sales representative upon request.
Choose between a split septum vs mechanical valve devices
With many devices available to practitioners, its important to note whether your device type is split septum or mechanical valve. These devices are also known as simple (split septum) or complex (mechanical) connectors.
Studies have shown that a split-septum needle-free connector is associated with a lower incidence of CRBSI’s compared to a mechanical valve device due to the latter having one or more moving parts in the fluid pathway.
Fluid Displacement Options
a) Neutral: Neutral displacement needle free devices are the dominant device used within the UK. These connectors do not generate ‘pressure’ or ‘force’ during fluid movement and prevents blood reflux moving into the catheter lumen upon connection and disconnection of IV sets or syringe.
Best practice specifies a needle-free device with neutral displacement as this prevents or reduces blood reflux (therefore reducing the risk of occlusion and CRIBSI’s).
b) Negative: The needleless devices that have a negative pressure fluid displacement
can cause the blood to be pulled back into the catheter lumen. If using a needleless connector with negative pressure, ensure to have a standardised clamping sequence in place for your points to practice and procedure guidelines.
Find out more about fluid displacement and blood reflux, with our video demonstration of negative pressure and neutral needle free devices. Watch here
c) Positive: Connectors with mechanical valves are designed to provide a positive fluid displacement upon disconnection of the IV set or syringe. Upon disconnection, the fluid in the valve is pushed out to the catheter lumen to remove the blood that has refluxed. Blood can still move in to the catheter dip, but the displacement valve prevents blood from staying inside.
However, ‘The Society for Healthcare Epidemiologists of America and Infections Disease Society of America have recommended against using positive displacement needless connectors’ This is due to reports of increased CRBSI’s using these devices, and ‘The FDA has received three reports of death associated with BSI and positive displacement needless connectors.’ (20).
Device & Septum Disinfection
When using a needleless device in practice, disinfection is a vital part of usage. Consider the following four points when introducing and/or changing your needless connector within your trust.
a) Disinfecting your Needless Connector: Epic3 recommends (IVAD 30) the use of 70% isopropyl alcohol with 2% chlorhexidine. The recommendation relates specifically to active disinfection (wiping the hub) and it is categorised as a ‘Class D/GPP’ recommendation. (21)
b) ‘Scrub the hub’: CDC guidelines also recommends to ‘scrub the hub’ with 70% isopropyl alcohol. This is a microbiologically driven recommendation, given the evidence with regards to known contamination and effectiveness of cleansing. (22)
c) Septum Disinfection: When making your device selection for your practice, also ensure to review the design of the connector for a smooth external septum surface with few, if any, gaps that can be more thoroughly disinfected (4)
d) Passive disinfection: Passive disinfection has been shown to provide statistically better outcomes in clinical practice than active disinfection as it eliminates user variation by delivering consistent needle-free device disinfection.
For more information on ANTT – Aseptic Non-Touch Technique see https://www.antt.org
Biofilm Reduction
The design of the needleless connector should, where possible, reduce opportunities for biofilm to develop. A core example of this is ensuring there is a tight seal between the septum and the needle-free connector housing to reduce or eliminate space for contamination to occur. (3,4)
Fluid Pathway Considerations
When reviewing your needless connector for your department, attention should be paid to the fluid pathway within the device. Assess your device on the three criteria below:
a) Direct, Straight Fluid Pathway: A direct, straight fluid pathway facilitates adequate flushing and reducing the internal space for potential biofilm development (3,4)
b) No moving parts: A needle-free device with the most direct and least tortuous fluid pathway, with preferably no moving parts aids in reducing the potential risk of CRISBI’s (4)
c) Minimised dead space: Within the device, a connector with little or no dead space in the fluid pathway minimises the surfaces that infusates can contaminate and where biofilm can develop (4)
Clamping Sequence Requirement and Standardisation
Clamping has been a standardisation in nursing practice for over 50 years as a safety precaution for patients to prevent blood reflux related issues. However, success of this practice relies on standardisation and completion of the process by all individuals.
a. Neutral Displacement Needless Connector: The recommended best practice specifies a needle-free device (neutral displacement) that removes the requirement of a clamping sequence to prevent blood reflux related issues.
Selecting a neutral displacement needle free connector reduces the need for clamping. Therefore, saving valuable time and effort of the departmental staff as well as reducing the potential for clinical error by removing the clamping requirement.
b. Standardisation of Needless Connector Valves: If you do not have a neutral-displacement needle free connector standardisation can be achieved by selecting one needle-free connector throughout the healthcare facility (either negative pressure or positive pressure).
This helps to streamline the training and standardisation process as healthcare workers understand and are well trained in the specific clamp-disconnection sequence. (4)
Device Design
a. Clear or Clearable: Studies suggest that a transparent needle-free connector is preferable to one that is opaque. As this give the practitioner better visibility of the fluid pathway within the device. However, this does depend on the personal preference of practitioners.
When considering needless connectors from Vygon, its important to note that although our our Bionector is non-transparent, flush studies have shown it is effective within the first 5mls of flushing solution.
b. Anti-reflux valves for Overdose Prevention: The MHRA (MDA/2010/073) recommends the use of anti-reflux valves on multi-lumen extensions, to prevent infusions backtracking and the risk of subsequent drug overdose. (18), when two ore more infusions are running simultaneously and at variants of pressure.
c. Application of Downstream clamps: The MHRA (MDA/2008/016) – Application of a downstream clamp to an IV line/catheter during positive pressure technique (to maintain catheter patency) may result in a recessed septum in some brands of connector due to the negative pressure generated between it and the closed clamp. Swabbing of the connector in this condition may lead to inadequate decontamination (19).
Compatibility with drug interaction and other IV Connections
Your needless connector is one part of your IV management system, so it is vital to ensure their suitability and compatibility. Considerations will need to be given to medication/drug compatibility, but also compatibility with other devices within your IV management for your department.
a. Drug Interaction and drug loss prevention: Adverse drug interactions with medical plastics is well documented. The material most frequently implicated with significant interactions is polyvinyl chloride (PVC). In the UK, syringe driver extension lines and IV catheters are made from plastics resistant to drug interactions, namely drug loss via adsorption, absorption, and permeation. (5-17). Ensure to select a needle free connector who’s tubing is resistant to drug loss.
b. Compatibility with other IV connections: The percentage of pre-filled glass syringe accesses vs the number of accesses for normal plastic syringes and IV extension sets is less than 1% of all accesses, which occur per year. Consideration should be given to why neutral displacement needle-free devise are the dominant device in use within the UK and what clinical benefits would be lost by changing to glass syringe compatible device on all types of IV Catheter. (21, 23)
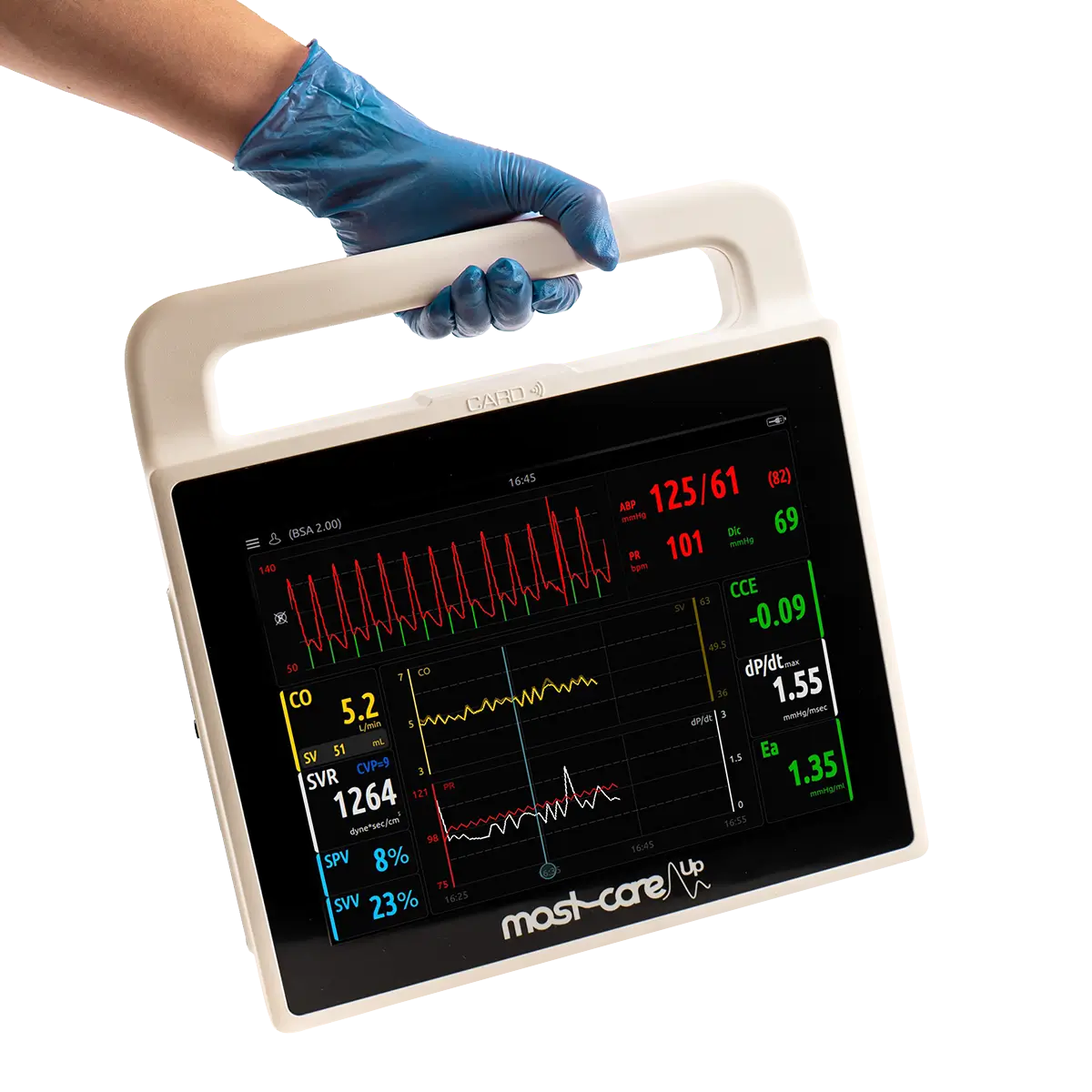
Clear benefits to patient and to staff
a. CRIBSI Reduction: Beneficial to patients and clinical staff, needless connectors helps to provide an effective barrier against microbial ingress to reduce catheter-related bloodstream infections.
b. Prevention of Needlestick Injuries: Using a needless connector is a vital part of iv management for any patient as it also reduces the risk of needle stick injuries and exposure to blood reflux.
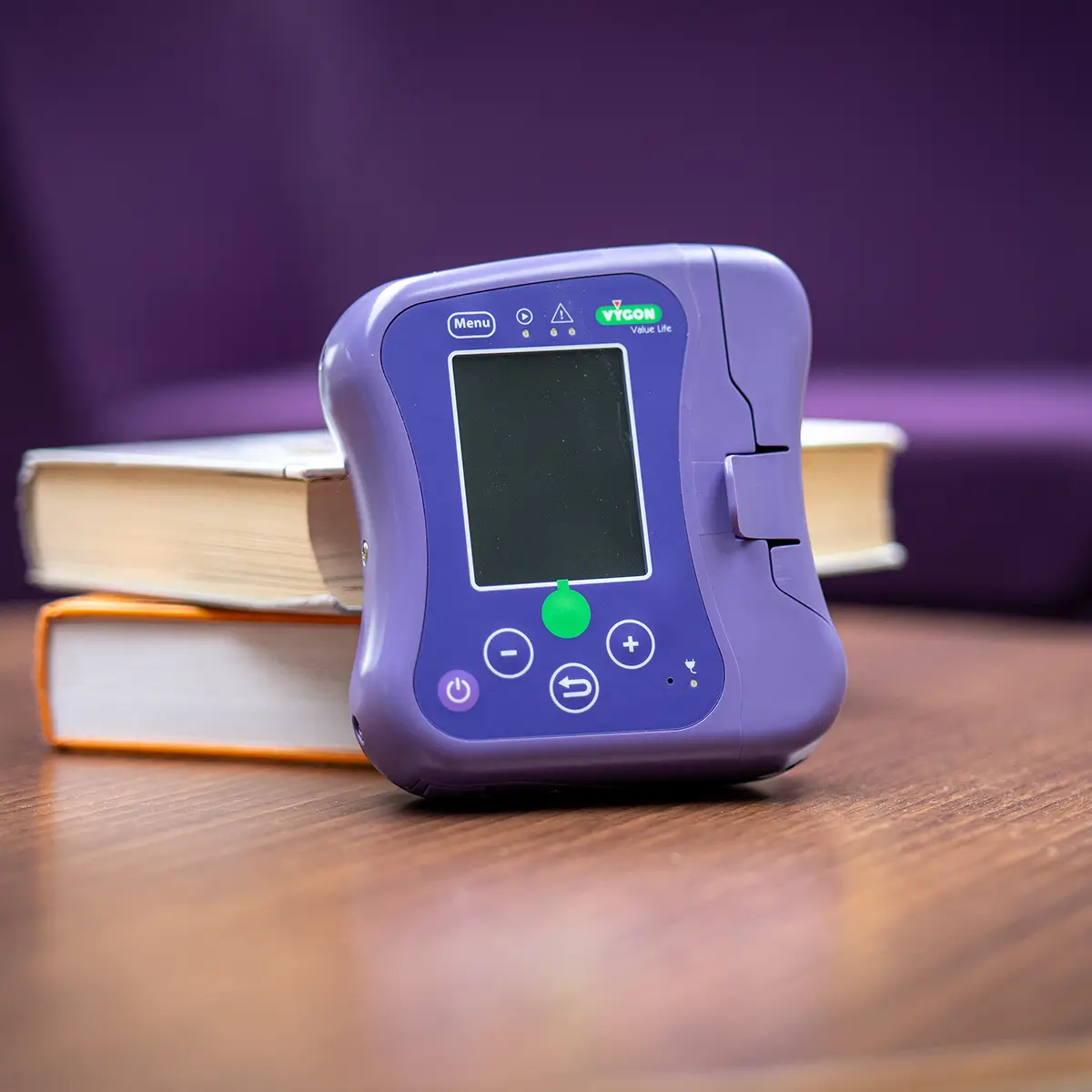
Needle free Connectors from Vygon UK
Here at Vygon UK, we offer three types of Needlefree Connectors:



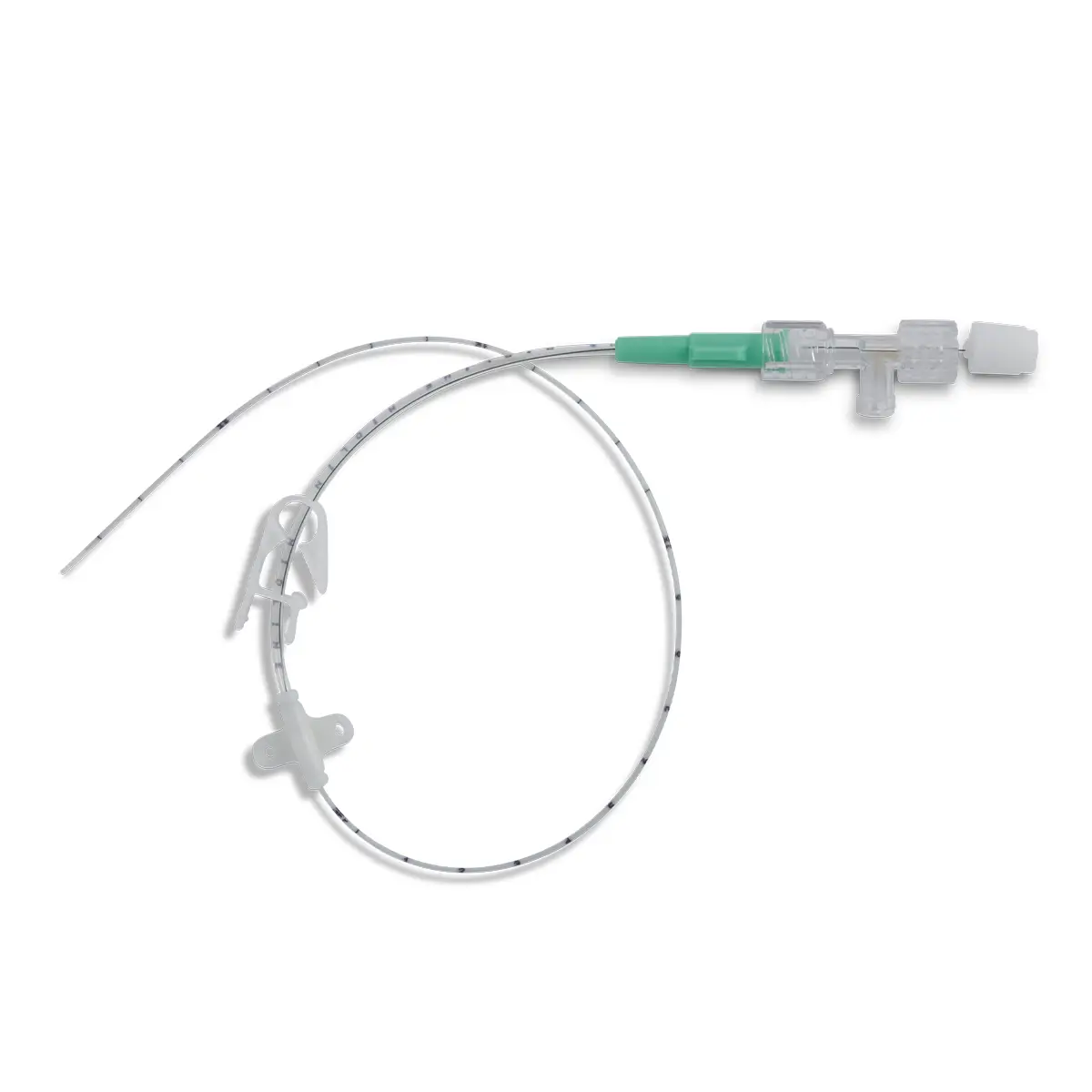
Bionector
- Market Leading
- Neutral Fluid Displacement
- Straight Fluid PAthway
- Wide range of Connectors
Find out more
Bionector TKO
- TKO: To Keep Open
- Bi-directional fluid
- Straight Fluid Pathway
- Reduce Occlusions by 88%*
Find out more
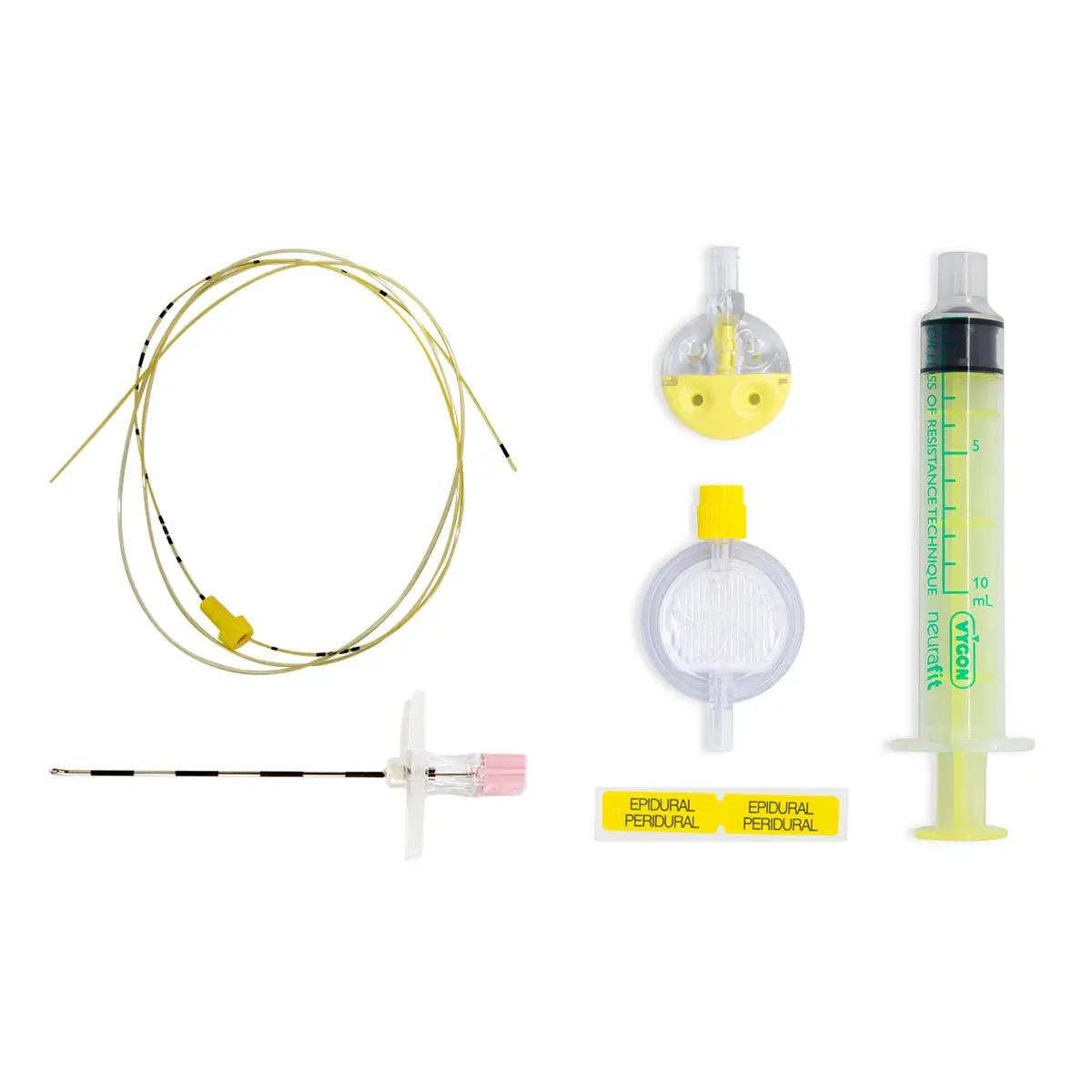
Vadsite
- Negative Fluid Displacement
- Straight Fluid Pathway
- Clear Housing
- Glass Syringe Compatible
Find out more
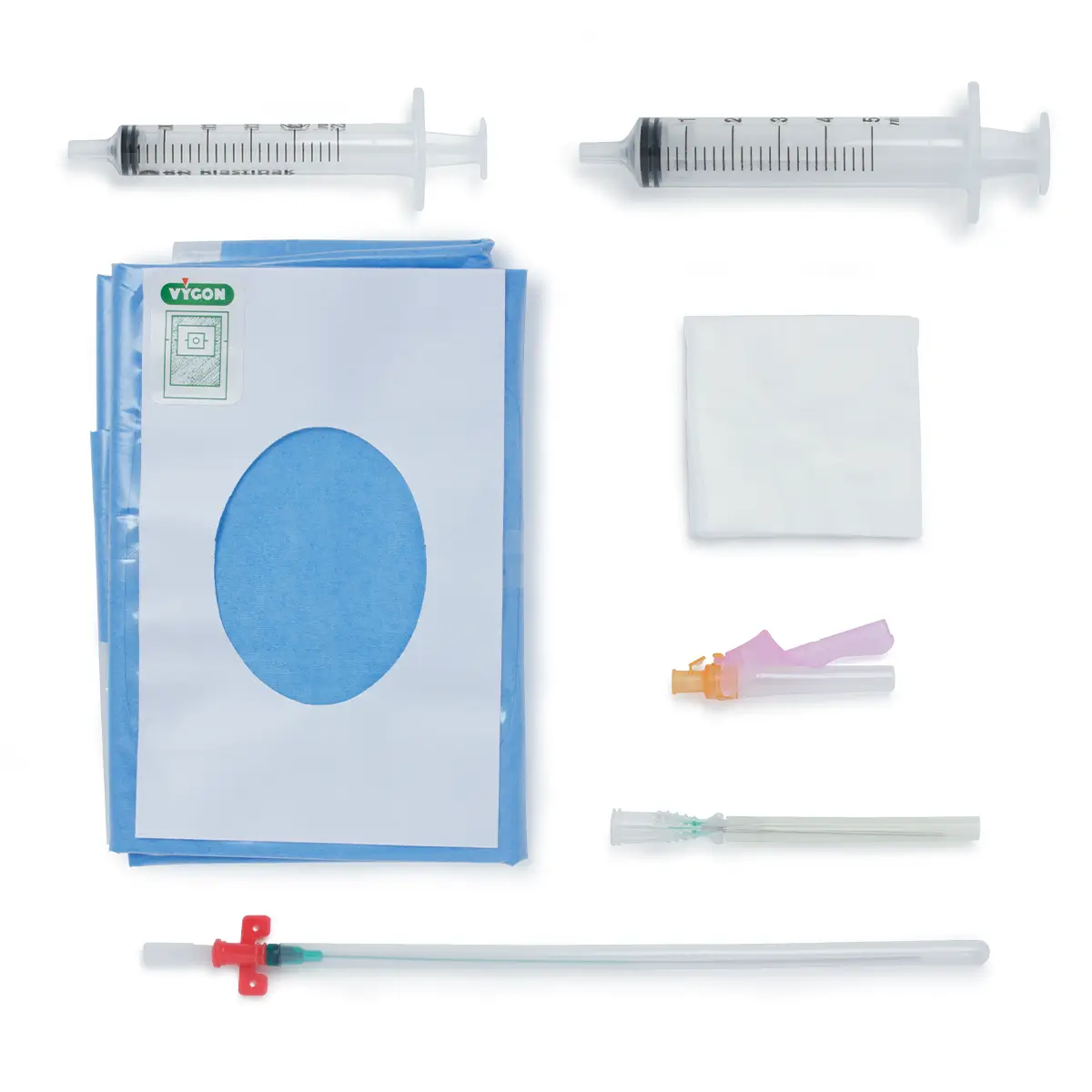
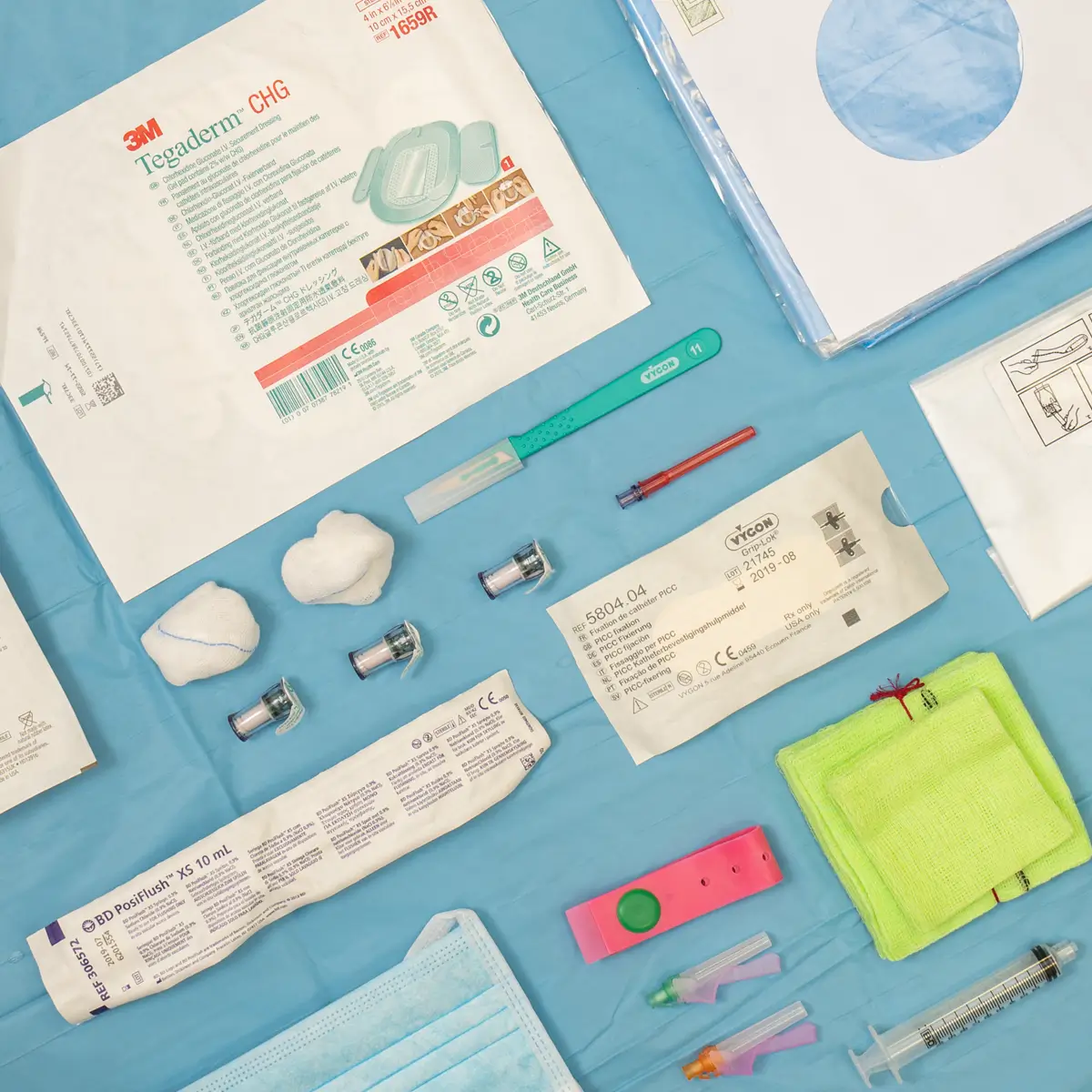
Total Solutions - The Vygon Difference
At Vygon UK we offer the Total Solutions package with all our needless connector devices. With a dedicated training and education program, combined with clinical tools, services, and solutions to support your healthcare professionals and patients.
References
Click the drop down to view references mentioned in the article.
Contact Us
To find out more about any of the Vygon Needless connector range, or to request a sample, please complete the form below, or give the Vygon team a call on 01793 748800