The benefits of antimicrobial impregnated lines in paediatric patient groups | CVCs

A brief review of two studies analysing the use of impregnated central venous catheters in paediatric patients and the effect on the rates of catheter-related bloodstream infections.
Keywords: antibiotics, antimicrobial impregnations, central venous catheters, bloodstream infection, paediatrics, rifampicin, miconazole.
Effectiveness of Impregnated Central Venous Catheters on Catheter-Related Bloodstream Infection in Paediatrics
The widespread use of CVCs has been shown to increase the risk of developing catheter-related bloodstream infection (CRBSI). PICUs are reported to have the highest rates of bloodstream infections with 1 in 10 children with a central venous catheter developing a central line-associated bloodstream infection8,9. Whilst there has been an increase in evidence to say that impregnated CVCs reduce bloodstream infections in adults and recommendations have been released, paediatric patients have had smaller studies and a large scale systematic analysis has not been conducted for this patient group.
A meta-analysis of available studies on impregnated CVCs used on paediatric patient groups was performed to evaluate the efficacy of central venous catheters impregnated with heparin and antimicrobial agents in comparison with standard and non-impregnated catheters on the prevention of CRBSIs (Catheter Related Blood Stream Infections). A total of six RCTs with 3,091 paediatric patients were included (with 1,781 patients for impregnated CVC intervention and 1,310 patients for standard CVC intervention). These patients were defined with the terms of being under the age of 18 with vascular catheters inserted for an expected duration of more than 72 hours.
Central venous catheters (CVCs) are clinically important in the treatment of venous pressure monitoring, infusion of drugs, and nutrient fluid supplementation (1). However, the widespread use of CVCs has been shown to increase the risk of developing catheter-related bloodstream infection (CRBSI) (2).
It has been reported that CRBSIs can occur in 13–20% of catheterized newborns by the Centers for Disease Control and Prevention (3) and that 1 in 10 children with a central venous catheter develops a central line-associated bloodstream infection (4). It is wellknown that CRBSIs increase children’s mortality, exposure to antibiotics, direct cost, and length of stay in the hospital (5, 6) 8
As well as comparing impregnated vs. non-impregnated catheters, the study collected and compared data on the agent in the impregnated CVCs. These included agents such as heparin, AgION, minocycline, miconazole, and rifampicin. Studies concluded that the agents most effective for paediatric patients were Minocycline; a second-generation, semisynthetic tetracycline, which effectively reduces the risk of CRBSI in paediatrics due to its antibiotic properties against both Gram-positive and Gramnegative bacteria; and the combination of Miconazole and rifampicin agents whose antimicrobial properties are estimated to reduce the risk of infections from 5% to 0%8.
Conclusion
By combining multiple existing studies, this systematic review concluded that the use of antimicrobial drug-impregnated CVCs had a significantly lower risk of CRBSI (RR = 0.48) than the conventional catheter group in the paediatric population8, making the implementation of antimicrobial drug-impregnated CVCs in PICU’s an effective anti-infection strategy in preventing CRBSI (p = 0.0002). The results were consistent with previous findings, but with more RCTs included for synthesized analysis, the results do provide more strength in increasing the statistical effectiveness.

The CATCH Trial
As well as the aforementioned systematic review, (Effectiveness of Impregnated Central Venous Catheters on Catheter-Related Bloodstream Infection in Pediatrics), a randomised controlled trial referred to as the CATCH trial, took place between Nov 2010 and Nov 2012 to assess the effectiveness of impregnated central venous catheters for the prevention of bloodstream infection in children admitted to 14 English paediatric intensive care units.
Patients were only eligible for the study if they were under 16 years of age and were expected to need a central venous catheter for 3 or more days.
Interpretation:
Antibiotic-impregnated central venous catheters significantly reduced the risk of bloodstream infections compared with standard and heparin central venous catheters. Widespread use of antibiotic-impregnated central venous catheters could help prevent bloodstream infections in paediatric intensive care units. 9
1,485 children were randomly assigned either standard, heparin-impregnated or antibiotic-impregnated catheters during the trial and results showed that bloodstream infections occurred in 4% of those with standard catheters, 3% in the heparin-impregnated group and 1% of the antibiotic-impregnated group.9
This study also came to the conclusion that antibiotic-impregnated catheters significantly lower the risk of catheter related blood stream infections in paediatric patients.
Enhanced Patient Safety with Antimicrobial Technology
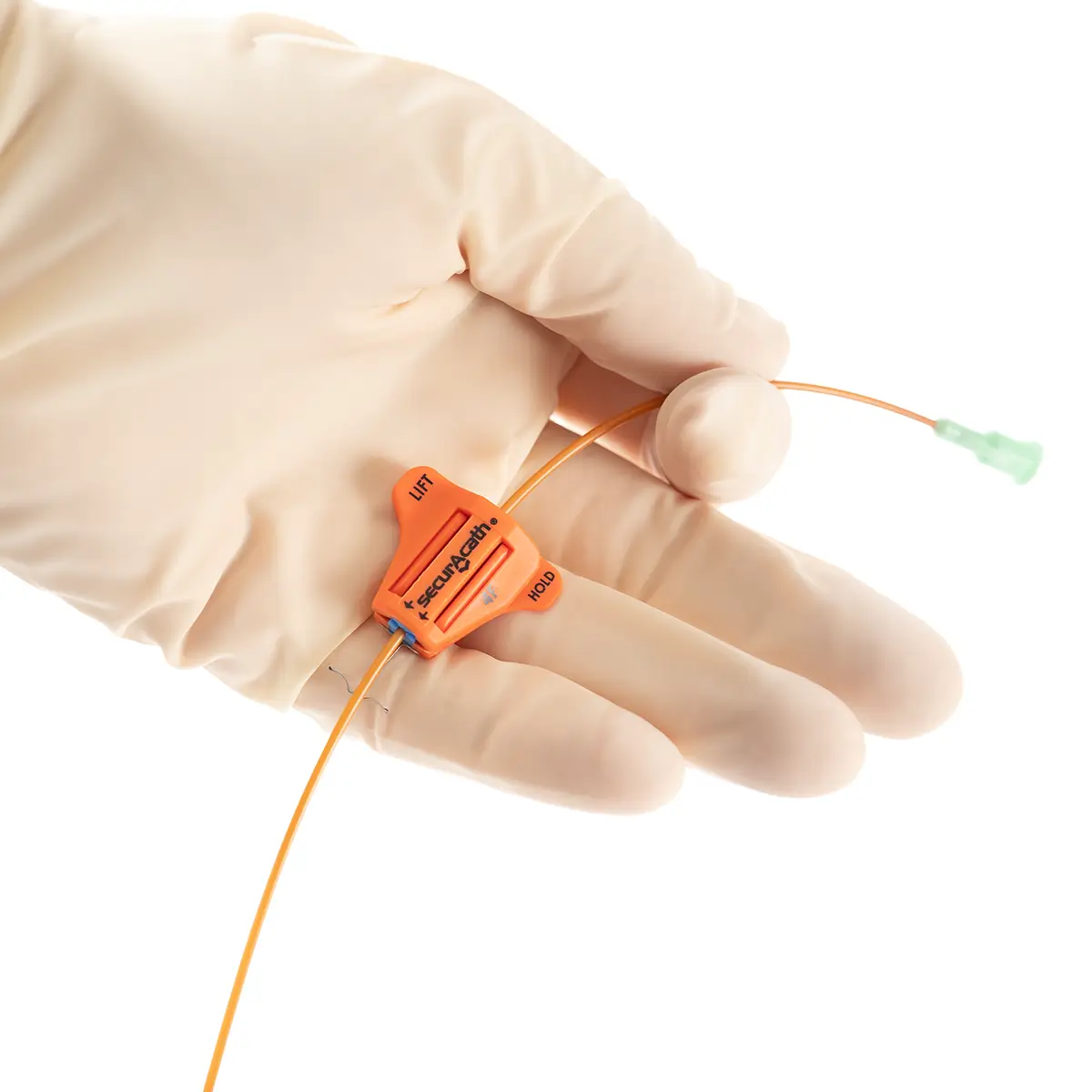
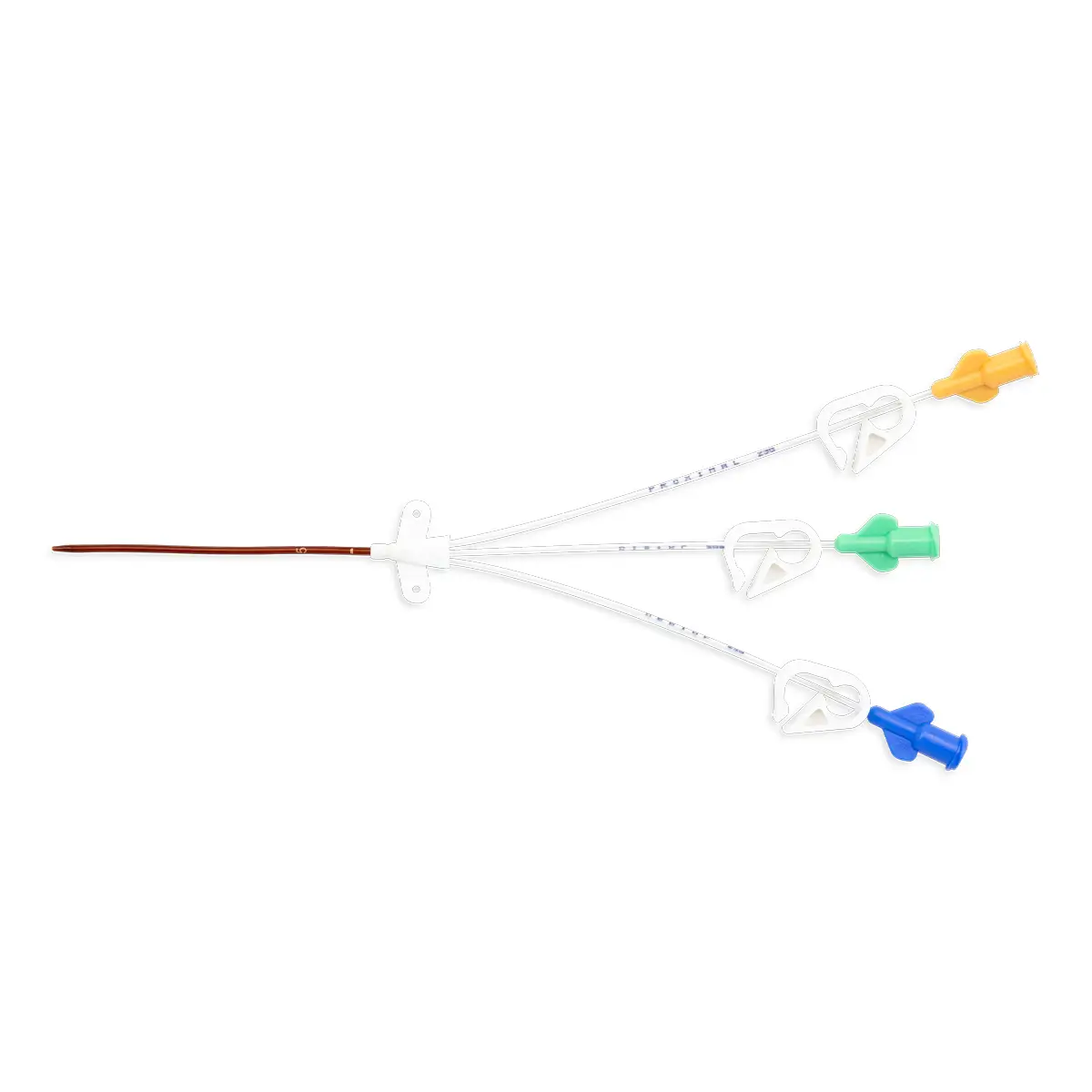
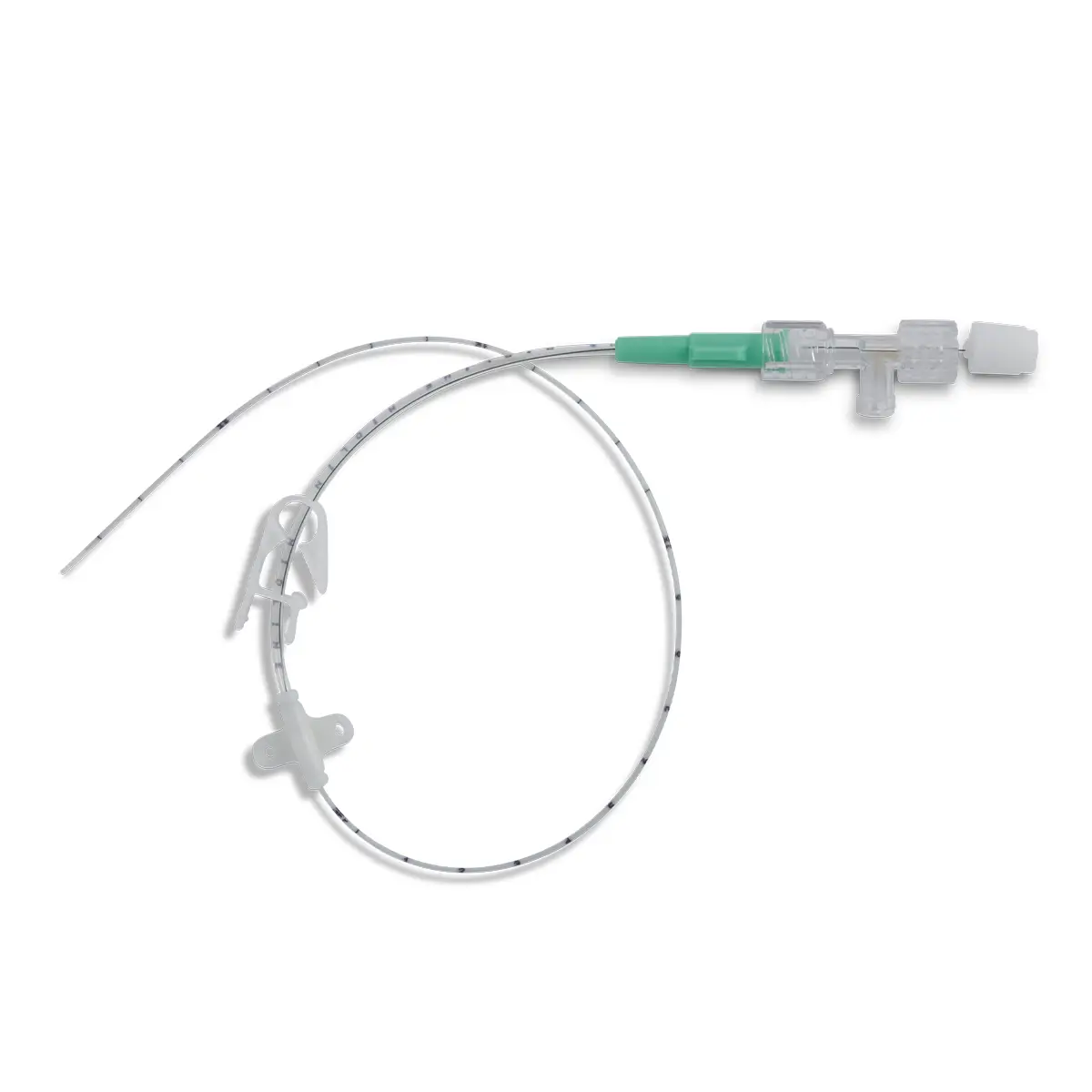
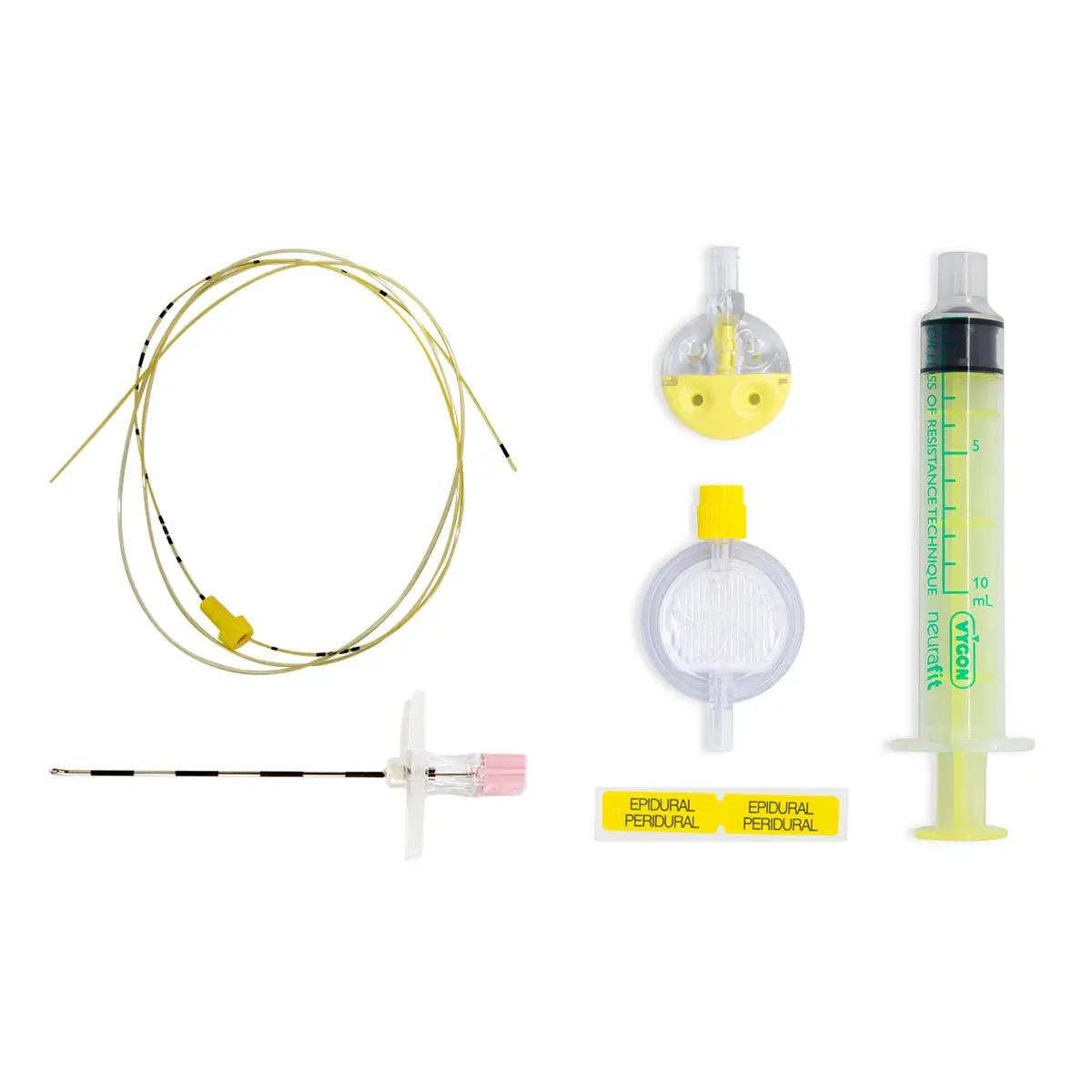
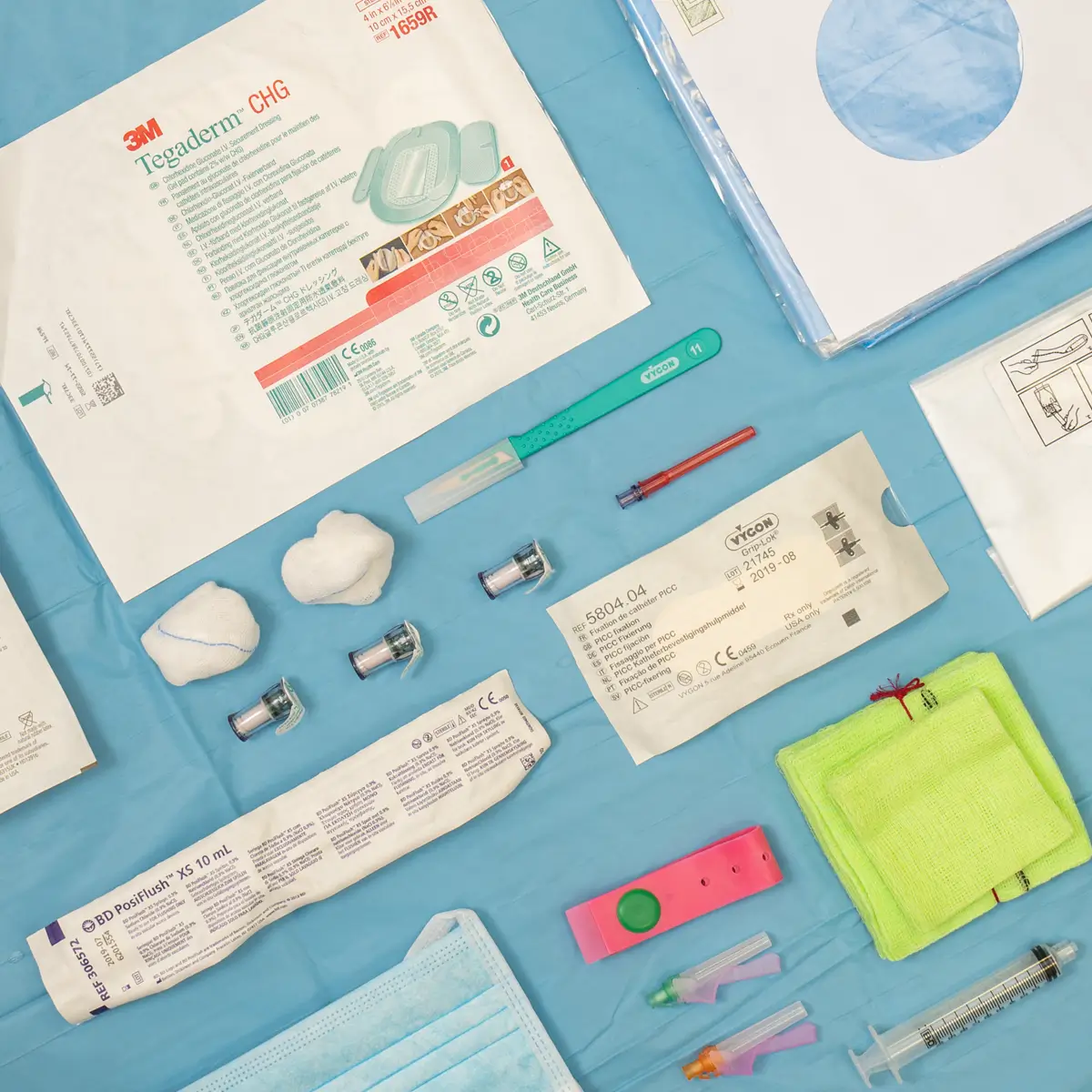
Vygon is the only supplier of a Rifampicin and Miconazole impregnated catheter, Multistar.
Multistar paediatric central venous catheter is specially designed for the treatment of paediatric patients.
Designed for enhanced performance and safety. Multistar incorporates the antimicrobials Rifampicin and Miconazole, to reduce the incidence of both catheter microbial colonisation and catheter related blood stream infections (CRIBSI’s).